Scoliosis is a side-to-side curve of your spine. This differs from your body’s natural front-to-back curve. It’s usually mild and doesn’t cause symptoms, but it can lead to back pain and abnormal posture. A healthcare provider most often diagnoses this condition during adolescence. Treatment includes physical therapy, braces and surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
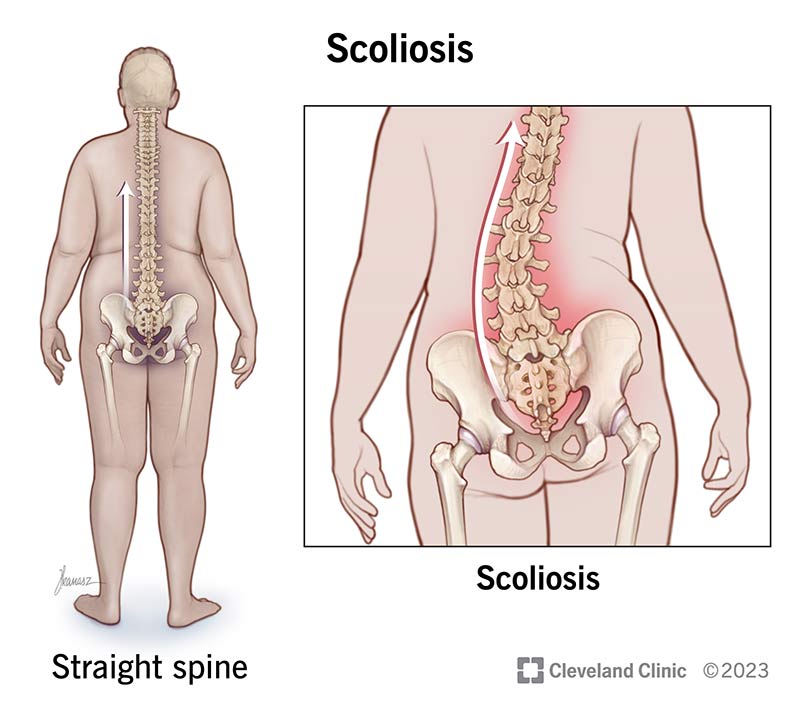
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15837-scoliosis)
Scoliosis is an abnormal side-to-side curvature of your spine. Your spine (backbone) naturally has a slight forward and backward curve. With scoliosis, your spine curves to the left and right into a C or S shape.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Most cases of scoliosis are mild, don’t cause symptoms and don’t need treatment. Severe cases can cause uneven posture and pain. Treatment may include wearing a brace or surgery.
There are three types of scoliosis:
You may hear your provider refer to scoliosis diagnosed during adulthood as adult-onset scoliosis or degenerative scoliosis. You may have had mild, undiagnosed scoliosis throughout your life. Symptoms can increase or appear as your body ages, which results in a late diagnosis. Specifically, adult-onset scoliosis happens when your disks and joints weaken or you lose bone density (osteoporosis).
Advertisement
Healthcare providers use different names to refer to idiopathic scoliosis according to when it’s diagnosed:
Scoliosis affects an estimated 2% of people around the world. In the United States, this equals over 6 million people.
Scoliosis usually doesn’t cause symptoms, but they may include:
Signs of scoliosis may include:
If you notice any of these signs, contact a healthcare provider for a screening.
Over time, you may notice:
Scoliosis can affect any part of your spine. There are some differences according to age:
The cause of scoliosis varies depending on the type but may include:
Most often, though, healthcare providers can’t identify a specific cause (idiopathic scoliosis).
You’re more at risk of developing scoliosis if you:
Scoliosis equally affects men and women. But women are more likely to need treatment due to the severity of the curve.
Is scoliosis genetic?
You’re more likely to develop scoliosis if someone in your biological family has the condition. But not all cases of scoliosis are genetic.
Without treatment, severe cases of scoliosis can lead to:
Contact emergency services if you have trouble breathing.
The first step of a scoliosis diagnosis is a scoliosis screening. You may remember getting a scoliosis screening during a pediatric wellness visit with your primary care physician or a school nurse. During a screening, a provider will ask you to:
Advertisement
A screening helps your provider look at your posture, alignment and spinal curvatures. If the physician isn’t your primary care provider, they may recommend you visit one if the screening indicates you may have scoliosis.
Scoliosis screenings happen during childhood and adolescence to detect scoliosis early. An early diagnosis can help your provider offer more treatment options, if necessary.
A healthcare provider will diagnose scoliosis after a physical exam. They may perform a screening in their office, which will include having you stand up straight and then bend forward to touch your toes. Your provider will examine your back to check the shape of your spine and see how you move around. They’ll also check your nerves by testing your reflexes and muscle strength.
Before your healthcare provider can suggest a treatment plan, they’ll ask you questions about the following:
Advertisement
If needed, your provider may order imaging tests. X-rays taken from the front and side will show a full picture of your spine. Your provider can then determine if you have scoliosis and if so, to what degree. Other imaging tests may include an MRI (magnetic resonance imaging) or CT (computed tomography) scan.
If your provider determines that you have scoliosis that requires treatment, they’ll refer you to an orthopaedic spine specialist.
A scoliosis diagnosis is most common during adolescence, between ages 10 and 15.
As you age, your spine curves (degeneration). For this reason, adults can get a scoliosis diagnosis later in life. This usually happens if scoliosis is mild and goes undetected during childhood.
A healthcare provider will measure the curve of your spine in degrees. They’ll rate the severity based on the degree of the curve:
This is similar to how you measure angles with a protractor in geometry class. Your provider will use a device called a scoliometer to measure the curve by placing the tool on your back. They may also order an X-ray of your spine to measure the curve.
Advertisement
Treatment for scoliosis isn’t necessary for all cases.
If your provider recommends treatment, they’ll consider several factors:
Treatment focuses on relieving symptoms and not necessarily straightening the curve. The goal is to decrease symptoms and curve progression and improve the function of your spine.
There are two types of treatment for scoliosis:
Most cases of scoliosis don’t require surgery. Instead, providers recommend conservative treatment first, which may include:
Your provider may recommend physical therapy. This can help you strengthen your muscles and relieve pain. Your physical therapist may help you with the following:
Surgery may be an option to treat some types of scoliosis that don’t respond to conservative treatment. Your provider may recommend surgery to:
There are different techniques your surgeon may use to treat scoliosis, including:
Advances in surgical techniques and computer-assisted technologies make less invasive approaches possible and recovery time quicker.
Are there complications of scoliosis surgery?
Scoliosis surgery is a safe procedure, but complications are possible and may include:
Though scoliosis is often asymptomatic, symptoms may appear as your body ages and natural spine degeneration occurs. A healthcare provider can help you manage symptoms if they become bothersome.
Scoliosis can change the way your body looks depending on the degree of the spinal curve. This might be challenging for your emotional well-being. A mental health professional can help you manage how you feel about your body.
The outlook for scoliosis can vary depending on the type and severity. Most people can live normally, without any changes to their routines.
There’s no known way to prevent scoliosis.
If you have scoliosis, a healthcare provider might recommend strengthening your back and abdominal muscles with stretching and exercises. These can help prevent the curve in your spine from getting worse.
Talk to your healthcare provider or physical therapist about what activities are safe to do. Most people with scoliosis can participate in physical activities and exercise. Routine movement can reduce the severity of symptoms. If an activity causes pain, listen to your body and stop.
Most cases of scoliosis are diagnosed during adolescence. This is the time when many children are eager to jump into team sports and athletic programs. As a parent or caregiver, you might wonder what activities are safe for your child.
Luckily, playing sports won’t make scoliosis worse. In fact, participating in sports that promote flexibility and core strength can reduce your child’s symptoms.
Sports that can help scoliosis include:
Should certain sports be avoided with scoliosis?
Talk to your child’s healthcare provider about what’s safe for them. Most sports, even weightlifting, are generally fine. However, if your child had back surgery, they should avoid contact sports. These include hockey, lacrosse, wrestling and football.
Contact a healthcare provider if:
As a parent or caregiver, it’s important to contact a pediatrician if:
You may be worried if your child comes home from school with a note that says a screening revealed possible scoliosis. Or maybe you visited your provider and they noticed bone degeneration that’s affecting your own posture and height. Most cases of scoliosis are mild, and treatment isn’t always required. Often, nonsurgical options, like wearing a brace, are all that you need. However, surgery is available and a safe option to treat severe curves. Your provider will let you know if they recommend treatment and give you advice on how you can take care of yourself or your child after a scoliosis diagnosis.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic offers minimally invasive treatments and surgery to correct posture and reduce symptoms that come with adult scoliosis.
