A liver transplant is a lifesaving operation to replace a diseased liver with a healthy one. You might need a liver transplant if you have liver failure or liver cancer. There are many people on the waiting list for a new liver. Those who meet the criteria to join the list are ranked by the urgency of their need.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
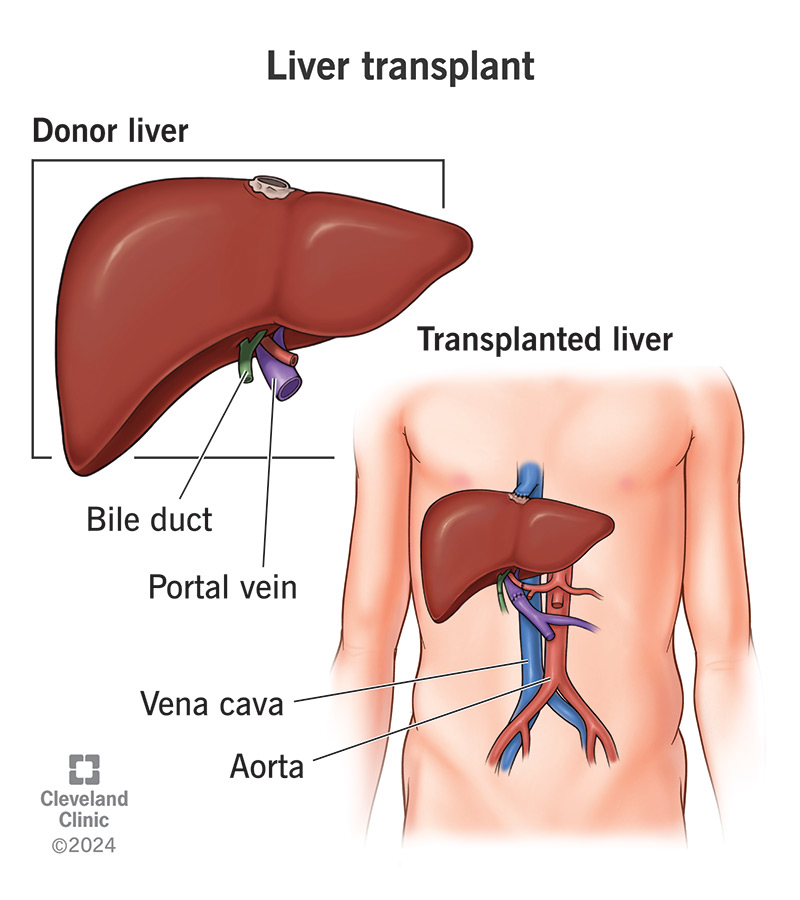
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/8111-liver-transplant.jpg)
Liver transplantation is surgery to replace a diseased liver with a healthy one. The healthy liver comes from either a deceased or living donor. You may need a liver transplant if you have liver failure or liver cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your liver performs many critical functions that keep you alive. If it becomes severely damaged, you’ll need a replacement to survive. If you meet the medical criteria for a liver transplant, you’ll be added to a U.S. national waiting list.
The wait can be long. There are far more people on the list than there are donor livers available. Each year, some people die or become too sick to have surgery while waiting for a transplant.
But surgery success rates are high. About 90% of people who have a liver transplant survive the surgery and recovery process, which can take up to 12 months. The current five-year survival rate is about 73%.
Liver transplantation is typically a last resort when your liver can no longer support your body. This may be because your liver is failing (losing its function) or because it has cancer that needs to be removed.
Conditions that may qualify you for a liver transplant include:
Advertisement
Your healthcare provider must also determine that you’re well enough to have organ transplant surgery and likely to recover. Certain medical conditions may make the procedure too risky.
Conditions that may disqualify you from having a liver transplant include:
If your healthcare provider recommends a liver transplant for you, they’ll refer you to a transplant hospital. A multidisciplinary team will evaluate you to determine if you’re a candidate.
Each transplant hospital has its own criteria for accepting transplant candidates. If they accept you, they’ll put you on the national waiting list maintained by United Network for Organ Sharing (UNOS).
To be a match for a donor liver, you’ll need to:
If you have acute liver failure with immediate need for a liver transplant, you’ll go to the top of the waiting list. Most people on the list have chronic liver disease, which tends to progress more slowly.
In those cases, UNOS uses a scoring system called MELD (Model for End-Stage Liver Disease) or PELD (Pediatric End-Stage Liver Disease). These scores are based on your blood test results to determine your place on the waiting list.
When a donor liver becomes available, your transplant coordinator will contact you and ask you to come to the hospital right away. Surgery will begin as soon as possible after both you and the liver have arrived.
While you wait, you’ll have standard screening tests to make sure you’re ready for the operation. You’ll also meet with your surgeon and anesthesiologist to go over the plan and prepare for surgery.
Liver transplantation is a major operation that can take up to 12 hours. You’ll receive general anesthesia, so you’ll be asleep through the procedure. You’ll also have several tubes in place to support your body throughout the surgery.
You’ll have:
Advertisement
During the operation, your surgeon will:
If you have friends or family waiting at the hospital, a member of your care team will check in with them throughout your surgery. They’ll let them know as soon as you wake up from the anesthesia.
If you have end-stage liver disease or liver cancer, a liver transplant is your best hope of survival. It can extend your life and significantly improve your quality of life.
Like any major surgery, liver transplantation comes with risks. These range from minor complications to serious ones that may affect your recovery or long-term health.
Complications from the procedure itself can include:
Advertisement
Complications after the procedure can include:
You’ll likely stay in the intensive care unit (ICU) for several days after your surgery. During this time, you’ll receive fluids and nutrition through an IV until your body is ready to handle liquids and solid food. You’ll also receive pain medication as needed.
Your healthcare team will monitor you closely and check for any signs of complications. They’ll take blood samples to see how well your new liver is working and may need to manage things like:
When your vital signs are stable and your new liver is functioning well, you’ll move out of the ICU to a regular hospital room. You’ll continue recovering there for another one to three weeks.
Before you go home, your care team will teach you how to:
Advertisement
In general, contact your care team right away if you experience:
Most people can return to work within three months and return to all other activities within six to 12 months. As you continue to recover at home, you’ll have frequent follow-up visits with your healthcare team.
The scar from open liver surgery is typically six to 12 inches long. It may run horizontally across your abdomen or be shaped like a “V.” The scar may appear red or brown and raised above the skin. In some cases, it fades over time; in others, it may remain visible.
After an organ transplant, you’ll need to take immunosuppressant medications for the rest of your life. You’ll usually start with a higher dose and then taper to a lower maintenance dose over time.
Immunosuppressants can cause side effects, so your healthcare team will monitor you closely with regular blood tests and adjust your medications as needed.
Common immunosuppressants include:
These medications work by suppressing your immune system to prevent it from attacking your new liver. But this also means your body will be more vulnerable to everyday infections and certain diseases.
Possible side effects of immunosuppressants include:
About 90% of people survive at least one year after liver transplantation, and nearly 65% are still alive after 10 years. Some people live for decades. However, many factors can affect your personal life expectancy, including:
Your healthcare provider is the best person to ask about your life expectancy and expected quality of life after liver transplantation. They know your medical history and current medical status.
You can take care of your new liver and your overall health by:
Your liver does so many vital jobs that no medical or mechanical substitute can replace it. Most of the time, you don’t even notice it working — until something goes wrong. When liver failure begins, its importance becomes clear.
Liver disease can have many causes. Some are out of our control, and others may go unnoticed until the damage is already done. When your liver starts to fail, a transplant may offer new hope — and a second chance at life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Hearing you need a liver transplant can be life-changing. But Cleveland Clinic is here for you with expert care that’s focused on you every step of the way.
