Peyronie’s disease is a condition in which scar tissue causes your penis to curve or lose length or girth. In some cases, it can cause pain and make it difficult or impossible for you to have sex. Causes may include an injury to your penis or a connective tissue disorder. A healthcare provider can diagnose and treat Peyronie’s disease.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
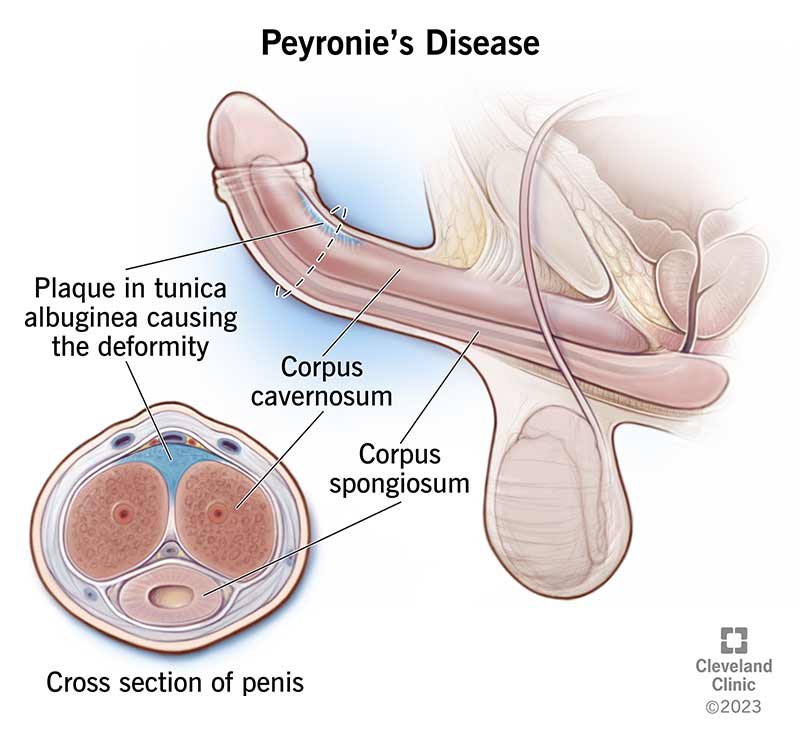
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/10044-peyronies-disease)
Peyronie’s (pay-roe-NEEZ) disease is a condition in which scar tissue (plaque) in your penis causes it to bend, curve or lose length or girth (circumference). You may be able to feel the scar tissue through your skin, or you may have pain in a specific part of your penis as the scar tissue forms. When you have an erection, your penis may bend up, down or to the side, depending on the location of your scar. Some people who have Peyronie’s disease don’t have a curve, but might have an indentation that gives their penis an “hourglass” appearance.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Most males don’t have perfectly straight erections. If your penis has a little curve — even if you’ve had the curve your whole life — it doesn’t mean you have Peyronie’s disease.
Peyronie’s disease has two stages: acute and chronic.
Medical experts estimate that about 6% to 10% of people between the ages of 40 and 70 with penises have Peyronie’s disease. It can affect anyone with a penis, but it’s less common at other ages.
Peyronie’s disease may be even more widespread because many people may feel too embarrassed to talk about it with a healthcare provider. It’s a good idea to talk to a healthcare provider any time you have concerns about your sexual health.
Advertisement
The primary symptom of Peyronie’s disease is a curve or bend in your penis. You may also be able to feel scar tissue under the skin.
Other symptoms of Peyronie’s disease include:
Peyronie’s disease symptoms may develop quickly or over a long period of time. Pain tends to decrease over time, but the bend in your penis can cause complications. If you have a bend in your penis greater than 30 degrees (which looks like when the hands of an analog clock read 1:00), it can make sex painful or impossible.
Yes, Peyronie’s disease can be painful. Pain most commonly occurs during the acute stage. But it may continue in the chronic stage. The severity varies from person to person.
In most cases, the scar forms on the top of your penis, causing it to curve upward when you have an erection. Your penis will bend downward if the scar is on the bottom and sideways if the scar is on the side.
In some cases, the scar develops on both the top and bottom of the penis shaft. This “dents” your penis and makes it shorter. In other cases, the scar goes all the way around your penis. This makes your penis narrow, like the neck of a bottle or the center of an hourglass. About 1 in 3 people who have Peyronie’s disease have calcium in the scar tissue. This can make your penis feel like a bone.
The cause of Peyronie’s disease isn’t always clear.
Some researchers believe scarring occurs after an injury to your erect penis — usually abnormal bending during sexual intercourse. However, up to 80% of people with Peyronie’s disease don’t remember a specific event that preceded changes to their penises. These changes may happen as a result of small, unrecognized injuries that occur during regular sexual intercourse. People who have Peyronie’s disease may have a higher risk of developing too much scar tissue in response to these small injuries.
Not all people who injure their penises get Peyronie’s disease, so there may be genetic or environmental factors that play into it.
No, Peyronie’s disease isn’t a sexually transmitted infection (STI) and it isn’t contagious.
Anyone with a penis can get Peyronie’s disease. However, the following risk factors may increase your chances of getting it:
Advertisement
Changes to your penis can affect your mental and emotional health. These may include:
Yes, Peyronie’s disease can cause erectile dysfunction. The penile plaque or scar tissue can interfere with how your penis stores an adequate amount of blood during erection. This results in an inability to get or maintain an erection that’s hard enough to have intercourse.
Yes, severe Peyronie’s disease can shorten your penis.
The amount of length that you lose depends on how severe your penile curve is. Severe Peyronie’s disease can decrease the length of your penis from 0.5 cm (about 50 sheets of paper stacked on top of each other) to 1.5 cm (about 150 sheets of paper).
It depends on the severity of your Peyronie’s disease. In some cases, you can have sex but it may be difficult or painful for you or your partner. The greater the curve in your penis, pain or degree of erectile dysfunction, the more difficult it is to have intercourse.
A healthcare provider can diagnose Peyronie’s disease. They’ll review your medical history and ask questions about your symptoms, which may include:
Advertisement
The provider will also conduct a physical examination. During the physical exam, they’ll feel the scarring in your penis. They may need to examine your penis when you have an erection. If necessary, they may give you an injection (vasoactive drug) that temporarily makes your penis erect.
A healthcare provider may recommend a penile duplex Doppler ultrasound examination to help diagnose Peyronie’s disease. An ultrasound is a type of imaging test that helps:
Ultrasound also allows providers to determine the best treatment for you.
Advertisement
There’s no single treatment for Peyronie’s disease that’s appropriate for every individual. In fact, you may not need treatment if Peyronie’s disease only causes a small curve in your penis that doesn’t hurt and doesn’t make it difficult to have intercourse.
Peyronie’s disease treatment options include:
These therapies utilize an external device, such as a vacuum erection device or traction device (RestoreX®), to gently stretch your penis and sometimes even bend it in the opposite direction of the curve. It encourages the scar tissue to break down and can:
Most people need to use the traction therapy device for several months to see improvement.
There are generally no long-term side effects of properly using a traction therapy device.
A healthcare provider may recommend medications you take by mouth (oral medications) or inject into your penis. Providers usually recommend medications if you have acute Peyronie’s disease or if you’re not sure if you want surgery. However, they rarely result in a straight penis.
Injection medications may include:
Oral medications may include:
It’s important to know that there aren’t any reliable studies that show that oral medications can effectively decrease penile curvature or Peyronie’s disease-related plaques. However, they may reduce your symptoms.
Healthcare providers only recommend surgery if you have severe Peyronie’s disease that makes it difficult or impossible to have sex. You should only have surgery if you’re in the stable or chronic phase of Peyronie’s disease, in which the scarring and curvature no longer progress and you haven’t had any pain for between six and 12 months.
Peyronie’s disease surgery options include:
It depends on the severity of your condition and what type of treatment you receive. A healthcare provider will give you an estimate on when you can expect to feel better after treatment.
Some mild cases of Peyronie’s disease go away without treatment. But it’s rare for severe penile curvature or plaques to go away on their own without treatment.
Your body is unique, and how it responds to Peyronie’s disease may be different from others. In mild cases, your symptoms may improve without treatment. In more severe cases, your symptoms may stay the same or gradually get worse.
If you have Peyronie’s disease, it’s important to remember that your symptoms may not be permanent, even without treatment. It also won’t physically affect any other parts of your body, including your ability to have a biological child (fertility). Treatments can help reduce or eliminate your symptoms.
It’s also important to remember that even with treatment, it may take weeks or even months before you see results. However, the earlier you start treatment, the better your of chances of improvement. Waiting to start treatment or for the pain to go away can be frustrating, especially if you’re not able to have sex.
As you get older, your erections may be softer, or it may be more difficult to maintain firmness. Softer erections are more prone to bending unexpectedly during sex, leading to injury. You and your partner can reduce your chance of this type of injury during sex through the following:
You may still get Peyronie’s disease even if you’re not sexually active. There’s no way to prevent Peyronie’s disease if genetics or autoimmune diseases are the cause.
The following tips can help you take care of yourself if you have Peyronie’s disease:
See a healthcare provider as soon as possible if you notice a curve in your penis — especially if it gets worse over time — or have any concerns about your sexual health.
Go to the nearest emergency room if you have Peyronie’s disease symptoms as well as:
No, Viagra can’t treat Peyronie’s disease. However, erectile dysfunction medications may help reduce your risk of injury, which can help prevent Peyronie’s disease.
Peyronie’s disease is a type of penile curvature. Some people have penile curvature at birth (congenital penile curvature or chordee). There’s typically no association between congenital penile curvature and penile plaque, scarring or injury, and the condition doesn’t change over time. You may not notice it until after puberty, when you start having more regular erections.
No, Peyronie’s disease isn’t cancerous and it won’t turn into cancer.
No, Peyronie’s disease won’t affect your ability to have a biological child.
No, Peyronie’s disease doesn’t affect your ability to pee. Talk to your healthcare provider if you have Peyronie’s disease and have problems peeing.
No, blood in your pee (hematuria) isn’t a symptom of Peyronie’s disease.
No, Peyronie’s disease isn’t deadly. It affects the size and shape of your penis, but it doesn’t affect the rest of your body.
Any symptoms that affect your penis can be alarming and embarrassing, especially if they involve changes to its size and shape. You may think your symptoms will go away on your own or if you ice the area. However, these symptoms are your body’s way of telling you that something is wrong. It’s important to talk to a healthcare provider. They can diagnose Peyronie’s disease and get you the proper treatment.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When scar tissue builds up in your penis, it can cause it to bend, curve or even get shorter. This common condition is called Peyronie’s disease.
