Takayasu arteritis is a rare inflammatory disease that targets your arteries. Inflammation causes your arteries to harden and narrow, making it harder for blood to flow through them. This can cause life-threatening complications. Medications can reduce the inflammation and the damage. This is a lifelong condition, but many people go into remission.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
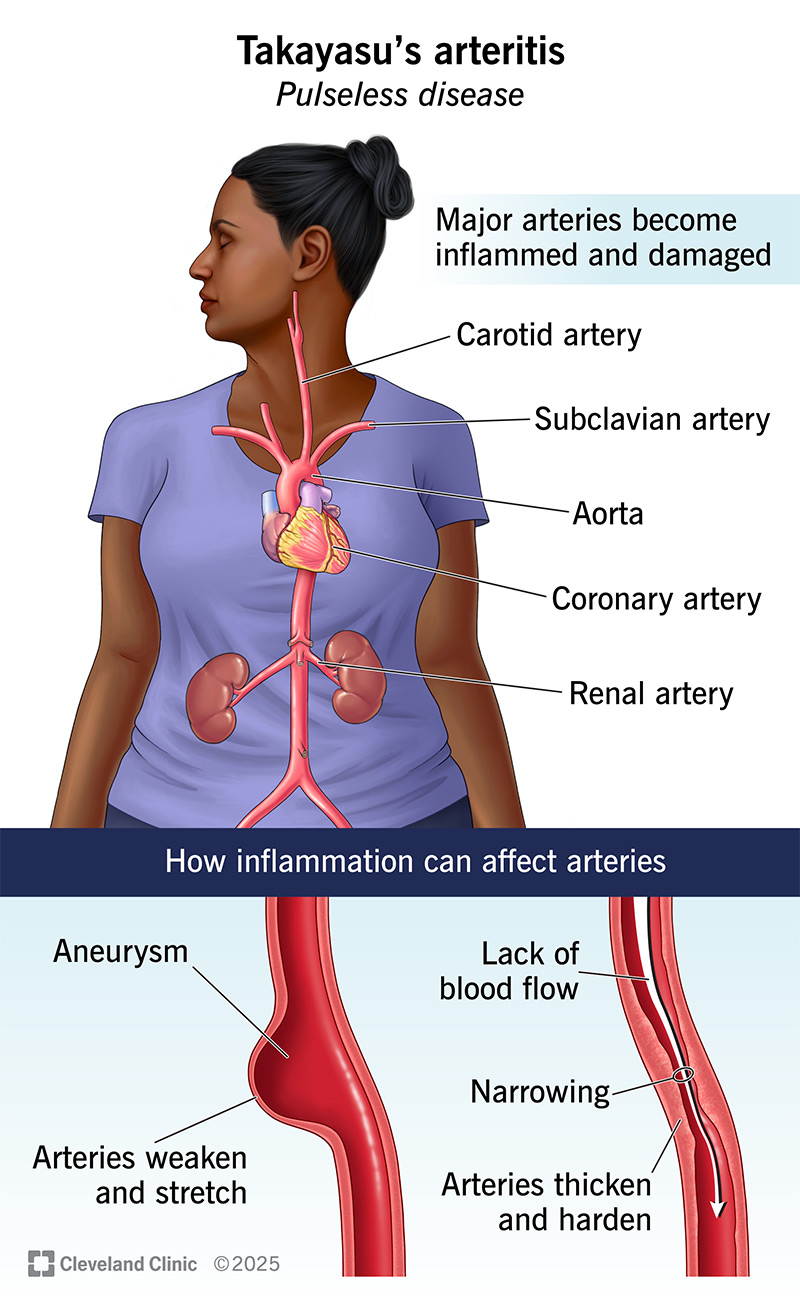
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/takayasus-arteritis)
Takayasu arteritis is a disease that damages your major arteries throughout your body. It’s a form of vasculitis, which is chronic inflammation in your blood vessels. Arteritis is inflammation in your arteries. These are the vessels that bring oxygenated blood to your organs and tissues. As Takayasu arteritis damages these vessels, it can reduce their blood flow.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Takayasu arteritis starts with general symptoms, like fatigue, loss of appetite and just feeling ill. Eventually, your arteries may become hardened and narrowed, which reduces their blood flow. Your blood flow through these arteries may become so weak that healthcare providers have difficulty finding your pulse. This is why it’s sometimes called “pulseless disease.”
Weak blood flow through your arteries (arterial insufficiency) can cause a variety of other symptoms and complications, some of which are life-threatening. It can affect your brain, heart, kidneys, limbs and other body tissues. It can also make daily life uncomfortable and difficult. Fortunately, once diagnosed, Takayasu arteritis is treatable, and it can even go into remission.
Chronic inflammation puts constant stress on your body. You might not notice this right away. But usually, the first symptoms you’ll notice will be vague symptoms of overall illness.
Early symptoms may include:
Since it’s a chronic disease, the inflammation never stops. Over time, it damages your arteries, restricting blood flow to your organs and tissues. This causes further complications.
Advertisement
Secondary symptoms can include:
Healthcare providers don’t know the exact cause of Takayasu arteritis. They believe it’s a type of autoimmune disease. This means your immune system attacks your arteries with inflammation by mistake. Inflammation is usually a tool for fighting infections. Some researchers believe an infection or toxin might trigger the process. Then, somehow, the inflammation continues on autopilot.
Takayasu arteritis starts in your aorta. This is the main channel that leaves your heart carrying oxygenated blood. From here, the inflammation spreads into your aorta’s major branches.
Chronic inflammation can have one of two effects on your arteries. It can weaken and stretch them, leading to aneurysms and bleeding. Or it may cause scarring that makes them thicken and narrow (stenosis). This constricts their blood flow. Sometimes, both of these things happen in different places.
Complications can include:
Takayasu arteritis is a rare condition. There are fewer than 2 million cases worldwide. It especially affects:
While it doesn’t seem to run in families, Takayasu arteritis does seem to run in ethnic groups. Researchers have recently identified several genes that might be connected with it.
Diagnosis of Takayasu arteritis is based on a combination of factors, including:
Advertisement
It can take some time to get the right diagnosis. Since the early symptoms of Takayasu arteritis tend to be mild and vague, you and your provider might not suspect it until you have more advanced symptoms.
Healthcare providers treat Takayasu arteritis with medications to control the inflammation and stop the damage to your arteries. Corticosteroids, like prednisone, are powerful anti-inflammatory medications. Most people start with corticosteroids and slowly reduce the dose as their condition improves. You might need to stay on a low dose, and/or take other medications, to manage your condition long term.
Other long-term medications may include:
Advertisement
While medications can limit further damage to your arteries, they can’t reverse the damage already done. Some people may need vascular surgery to restore blood flow to their organs and tissues.
These procedures may include:
Since Takayasu arteritis is a lifelong condition, you’ll need lifelong care, even if you’re feeling well. Your provider will monitor your condition regularly to make sure your treatment plan is up to date. Even when it’s working, you might have times when you feel better or worse. Taking stock of how you feel and letting your provider know can help them identify new complications or treatment side effects.
When you have Takayasu arteritis, it’s important to see your provider regularly so they can monitor your condition. You should also be sure to contact them if any new symptoms appear.
Talk with your provider if you become or plan to become pregnant. It’s possible to have a successful pregnancy with Takayasu arteritis, but it’s important to know how to manage it safely.
Advertisement
Seek emergency care if you develop:
Without treatment, Takayasu arteritis can be debilitating or even fatal. But with the right diagnosis and treatment, the prognosis (outlook) is good. In the United States and Japan, only about 3% of people with Takayasu arteritis die from it, after an average period of five years. Other parts of the world may have worse outcomes, due to low recognition of the disease, delayed diagnosis or poor access to care.
While there’s no cure for Takayasu arteritis, it usually improves with treatment. Symptoms may seem to come and go. When they’re active, you may find it hard to keep up with your usual activities. But after several years of treatment, many people find that their symptoms seem to go away for good. This is called remission. In this case, you may be able to stop treatment, although you’ll still need checkups.
Takayasu arteritis is serious, but it’s treatable. Once you get the right diagnosis and treatment, you can start to feel better. Over time, your symptoms may change or come and go. This is why it’s important to have a trusted provider to follow up with. Don’t be afraid to speak up if you notice something different about your health. Your provider will want to know about it so they can help you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic provides accurate diagnoses and personalized treatments for all types of autoimmune disorders, including lupus, MS and rheumatoid arthritis.
