A thymectomy is a surgery to take out your thymus gland. Most people who need this operation have myasthenia gravis or a tumor. Surgeons can use open or minimally invasive methods for a thymectomy. Pain after a thymectomy is often mild and the recovery is quick. However, it can take a year or more for people with myasthenia gravis to see results.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
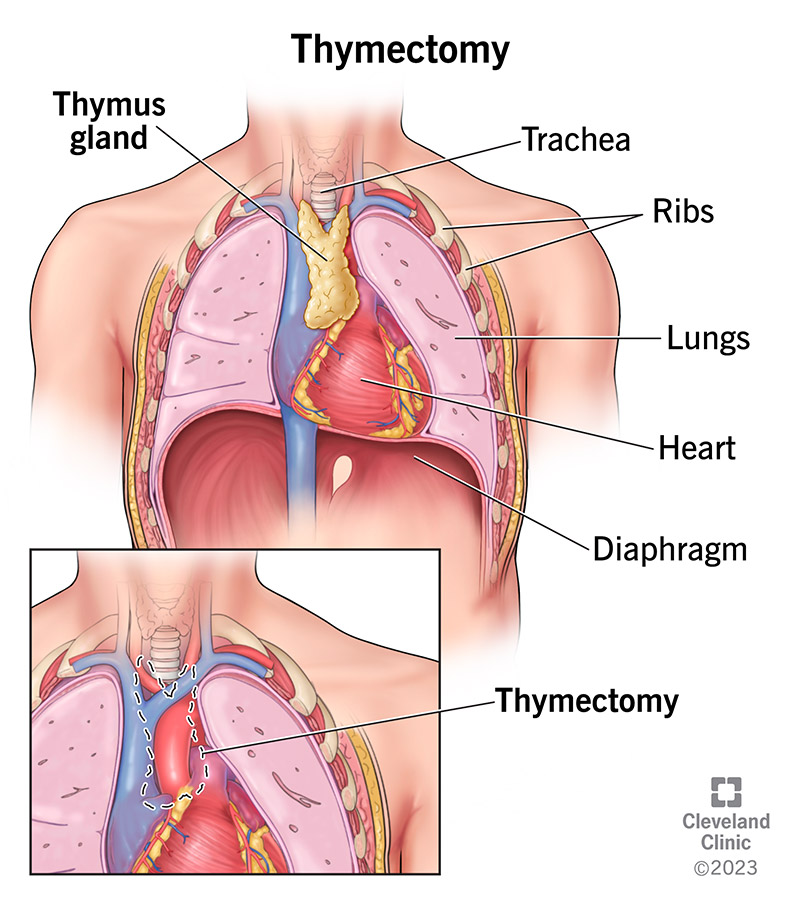
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/25041-thymectomy-illustration)
A thymectomy is a surgery to take out your thymus gland and thymic tumors. It’s in your upper chest in front of your heart. Surgeons can use several different approaches for thymectomy. Factors involved in the choice of method include your body mass index (BMI), prior surgery or disease treatment involving your chest, and the size of your thymus.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Thymectomies are rare procedures. One study reported that surgeons performed 7,000 thymectomy procedures in the United States during a 13-year period. Surgeons currently perform about 1,000 thymectomies per year in the U.S.
A thymectomy treats problems with your thymus gland, such as:
Before a thymectomy, a provider will review your medical history and do a physical exam. They may also order the following tests:
Anyone having a thymectomy should talk with their provider about whether to stop taking certain medications or supplements before surgery. Only stop taking medicine if your provider tells you to.
You’ll most likely need to stop eating and drinking at midnight before your operation.
If you have myasthenia gravis, you may need the following before surgery to prevent breathing issues:
It’s very important that people with myasthenia gravis do not stop taking their regular myasthenia gravis medications unless their physician (generally an anesthesiologist or surgeon) explicitly tells them to do so.
Advertisement
Healthcare providers can perform a thymectomy using open or minimally invasive ways that use cameras and/or robotic arms. Talk with your provider about which approach is best for you.
Thymectomy surgery steps include:
Thymectomy surgery steps include:
The length of time for a thymectomy varies depending on which method the surgeon uses and the difficulty of the clinical scenario. A thymectomy could take two to four hours.
After a thymectomy, you’ll be in a recovery room after a provider takes out the breathing tube in the operating room. You’ll need oxygen, fluids and pain medicines initially. Usually, a provider will transfer you to a regular room that same day of surgery.
People with myasthenia gravis who have a thymectomy have:
If you had a thymoma, thymectomy can often cure this usually slow-growing cancer.
Compared to open procedures, minimally invasive approaches can give you:
The majority of people who have a thymectomy for myasthenia gravis see benefits within a year of their operation.
Thymectomy side effects or complications may include:
Advertisement
Recovery time varies depending on whether you had open or minimally invasive surgery. Most people stay at least one night at the hospital. Depending on your particular situation, you might need a little more time to heal in the hospital after surgery. Although it’s very treatable, pain from your surgery should go away in two weeks.
One year after surgery, a provider will determine the benefit of thymectomy for myasthenia gravis. Most people don’t see an immediate benefit.
Follow-up appointments with your neurologist will help them decide how long to continue your medications for myasthenia gravis. Generally, they do this by lowering doses slowly over time based on your degree of symptoms.
The prognosis for thymoma varies by stage:
The right time to go back to work or school is different for everyone. People who have myasthenia gravis may have fatigue that keeps them from going back to regular activities right away. Also, people who do a lot of standing or lifting in their jobs will need more time to recover than someone with a desk job.
Advertisement
After a thymectomy, contact your healthcare provider if you have:
Most people don’t have surgery often, but it’s good to remember that surgeons perform surgery every day. They want the best results for you, so don’t be afraid to ask questions about your procedure. Because surgeons can choose from several different approaches to a thymectomy, you can get peace of mind from understanding why they recommend one over another for you. Whether a thymectomy is minimally invasive or not, the pain afterward is brief and very manageable with oral pain medications.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.