Ventricular assist devices (VADs) can offer a lifeline to people whose hearts are too weak to meet their needs. These tiny implantable pumps help circulate blood. After a surgical implant procedure, most people experience notable symptom improvement and better quality of life that lasts for years.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
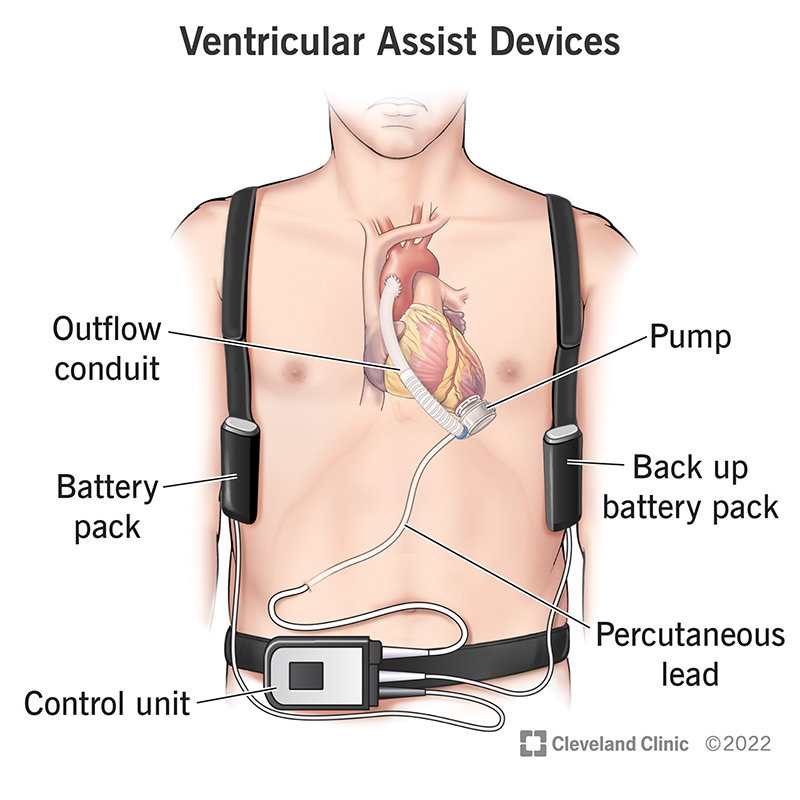
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22600-ventricular-assist-devices)
A ventricular assist device (VAD) circulates blood from a chamber of your heart (ventricle) to the rest of your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There are many types of VADs:
You might need a VAD if you have advanced heart failure and are either waiting for a transplant or require permanent help for your heart to circulate enough blood to your body.
Ventricular assist devices can help you in many ways:
Advertisement
The device has several components. Some are implanted and connected to your heart. Others stay outside your body.
Not everyone with severe heart failure is eligible for a ventricular assist device. Once you’re diagnosed with advanced heart failure, you have comprehensive medical and psychological evaluations. This may include assessing current heart and end-organ function. Healthcare providers screen for complex health issues such as breast cancer, prostate issues and infectious diseases. Additional tests include:
Evaluations also include discussions about living with a VAD as well as detailed education for basic day-to-day tasks of caring for the VAD. Your care team will also work with you to identify loved ones or a support system that you may live close to who will be able to help you, if necessary.
Here’s what happens during VAD implant surgery:
Advertisement
Many people notice:
Potential complications associated with the surgical implantation of a VAD as well as the lifelong usage of the VAD include:
VADs are not appropriate for some people, including if you:
After implant surgery, you’ll spend at least a few days in the ICU. Once you’re healthy enough to not need ICU-level care, you’ll transfer to the cardiac step-down unit for the rest of your hospital stay.
During your postoperative stay, healthcare providers will monitor your organ functions including your heart, kidneys, brain, lungs and liver. You’ll also work with physical and occupational therapists and other specialists as you learn to live with the new device. Your providers will prescribe a blood-thinning medication called warfarin sodium (Coumadin®) to take to keep your blood from clotting inside the VAD.
Advertisement
A nurse or VAD coordinator teaches you how to take care of your ventricular assist device. This includes how to:
Living with a VAD does come with some limitations, including:
Living with a VAD may include responsibilities such as:
Advertisement
Some people on ventricular assist devices experience depression and anxiety. You don’t have to deal with these feelings on your own. If you are struggling with these issues, it’s important to let your healthcare provider know.
Living with a ventricular assist device requires lifelong follow-up care. After discharge, you’ll visit your provider routinely. These visits will be more frequent at first. As you continue to improve and start to become more independent, your visits will become less frequent. Follow-up appointments enable your team to optimize your care by preventing, screening for and treating complications.
These visits may include:
Contact your healthcare provider if you have any questions or concerns or experience complications, such as:
You should also contact your healthcare provider if you notice issues with your VAD, such as:
Ventricular assist devices are mechanical pumps that take over your heart’s pumping action. They are for people whose hearts are too weak to meet their needs. A VAD can bring notable positive changes to your life including an increase in survival and an improved quality of life. For the best results, it’s essential to take good care of yourself and the device.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.