A urostomy is a surgery that creates an alternate way to let urine (pee) out of your body. It allows urine to exit through a stoma (opening) in your belly. This is helpful if you’ve had your bladder removed or have damage to other parts of your urinary system.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
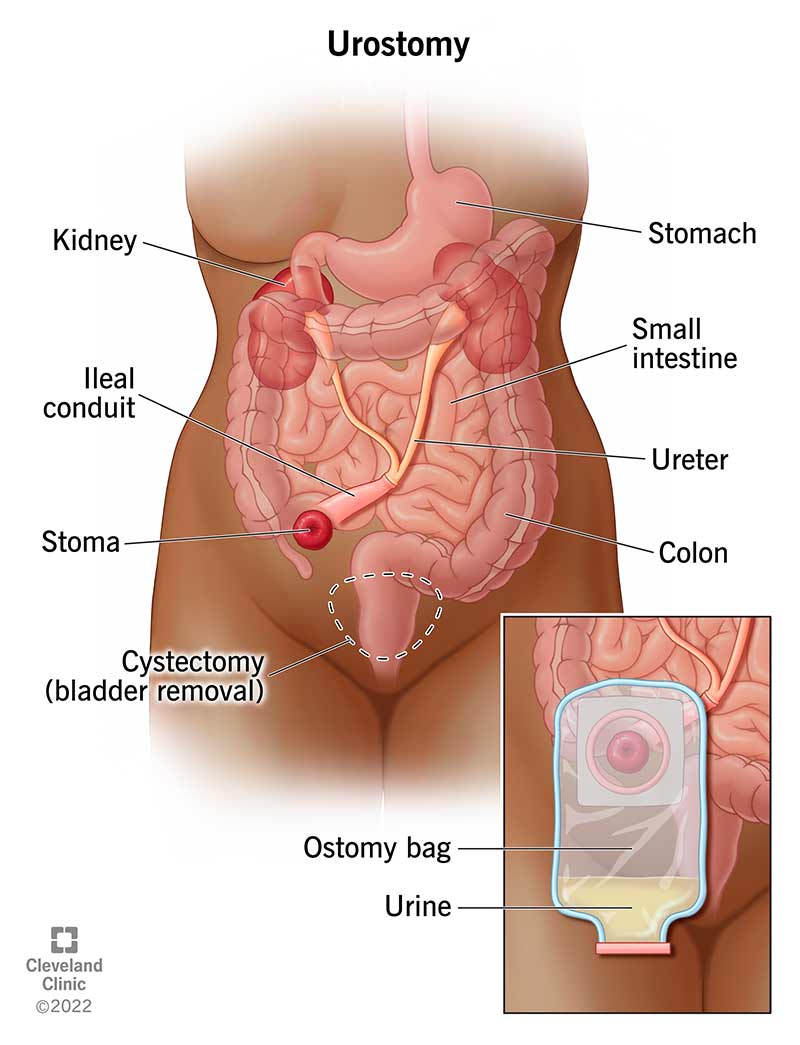
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/urostomy)
A urostomy is a type of ostomy surgery that creates an opening (stoma) in your abdomen for urine (pee). This opening allows urine to leave your body in a different way (urinary diversion).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A surgeon attaches the stoma to a place in your urinary tract to let urine leave your body. You use a pouch, also called a urostomy bag, to collect the urine for disposal.
In almost all cases, a urostomy is a permanent procedure that you can’t reverse. Your healthcare team can help you adjust to this change in how you live day to day.
You may need a urostomy for various reasons, like:
In all cases, a urostomy works by creating a different way for urine to leave your body.
There are different types of urostomies. They sometimes get their names from the way they create an alternate route for urine. They usually involve a stoma that constantly drains urine into a bag.
Your surgeon will use a piece of your small intestine to make a tube that will connect to the stoma. They typically use the tail end of your small intestines, or the ileum. This is why it’s called the ileal conduit. They’ll connect the newly created tube to your ureters, which drain urine from your kidneys. The urine flows through the tube to the stoma and then out of your body. The stoma will usually be on the right side of your belly.
Advertisement
This type of urostomy is similar to an ileal conduit. The difference is that your surgeon will use tissue from your sigmoid colon to create the tube.
In a ureterostomy, your surgeon will connect one or both of your ureters directly to a stoma in your belly. There is no segment of intestine in between.
Your healthcare team, including your surgeon, will speak to you before your surgery. They’ll make sure you understand:
Your team will give you specific information about not eating or drinking before your surgery and whether you should or shouldn’t take your normal medications. Make sure you tell your team about every type of medication and supplement you take.
Before the surgery, you’ll meet with your providers to find the best spot on your belly to place the stoma. The spot should be flat and easy for you to reach.
The details depend on the type of procedure you have. The surgeon will create the stoma in your belly at the site you chose. The surgeon will attach the ureters to the tube leading to the stoma.
You may need to have bladder surgery at this time to remove part or all of your bladder. Your surgeon may have to remove other organs, like your appendix, lymph nodes or parts of your reproductive system. (This may include the prostate in men or the uterus in women.) This is especially true in cases of cancer.
Your surgeon will perform the urostomy surgery while you’re under general anesthesia. You won’t feel any pain.
The surgery could last as long as six hours.
If you’re having a urostomy surgery, it’s because you’ve had problems with parts of your urinary tract. The urostomy can make your life easier.
Generally, a urostomy procedure is very safe. But risks with any type of surgery include:
Later complications could include:
After a urostomy, you can expect to:
After a urostomy surgery, some people leave the hospital after three days. Others stay as long as seven days, or even longer. During this time, you’ll learn about urostomy site care and how to use the necessary supplies (urine bags).
Advertisement
After you come home from the hospital, you’ll still need about two months before you go back to work or school. During this time, you can practice becoming more comfortable with using a urostomy bag (pee bag).
Meeting with a healthcare provider every month or so for the first six months after surgery can help you get answers to questions that may come up.
You should call your healthcare provider if you have any concerns about your urostomy. Call if you have:
Because a urostomy is usually long-term or permanent, you’ll need care for years to come.
Life expectancy after a urostomy varies from one person to another. People get urostomies for different reasons. Some are more serious than others. Talk with your provider about your prognosis in relation to the medical conditions you have.
You’ll still be able to get rid of urine, but it won’t be in the way you did it before. If you have an ileal or colonic conduit, you’ll drain urine continuously into a bag attached to the stoma.
When you look at your stoma for the first time, it might look a little bit bruised, red and swollen. This should change over time. The stoma will get smaller and lighter in color. The stoma will look like an oval or a circle, and it may stick out a little or be flat against your skin. It may look a little different from person to person.
Advertisement
The wound may hurt a little while it’s healing, but it’s your belly that hurts, not the stoma. You can use over-the-counter pain medications to manage it temporarily. The stoma itself has no nerve endings and doesn’t have any sensation. Once the surgery wound heals around the stoma, you won’t feel it.
You might have a variety of feelings about having a stoma. You might worry about how other people in your life will feel about it. A provider can help talk you through this. They can also connect you with urostomy support groups or other healthcare professionals.
You’ll need to empty your urostomy bag (pouch) about as often as you went to the bathroom before your urostomy. This could be every couple of hours or a little longer, but it could be more often if you drink a lot of fluids.
It’s best not to wait until the bag is full, so you should empty the pouch when it’s filled halfway or a third of the way. Leaking could cause emotional distress and irritate your skin.
You can connect your pouch to a larger drainage container so you’ll be able to sleep through the night.
How often you change the pouch depends on the type of system you’ve chosen. You’ll change some bags daily. Others are designed to last about three days or about a week.
Advertisement
Life after a urostomy will be different in some ways. It may take some time to get used to this change in your life and deal with feelings about your urostomy. Talk with your healthcare provider about any concerns you have. Seek out a support group if you want to talk with others who’ve had a urostomy. They can relate to what you’re experiencing.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
If you have a condition that’s affecting your urinary system, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
