If you have surgery on your lower abdomen or pelvis, your healthcare team might place you in the Trendelenburg position. It’s a tilted, head-down position that allows your upper organs to drift up and away from your lower organs, giving your surgeon better access. Besides surgery, there are a few other medical purposes for the position.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
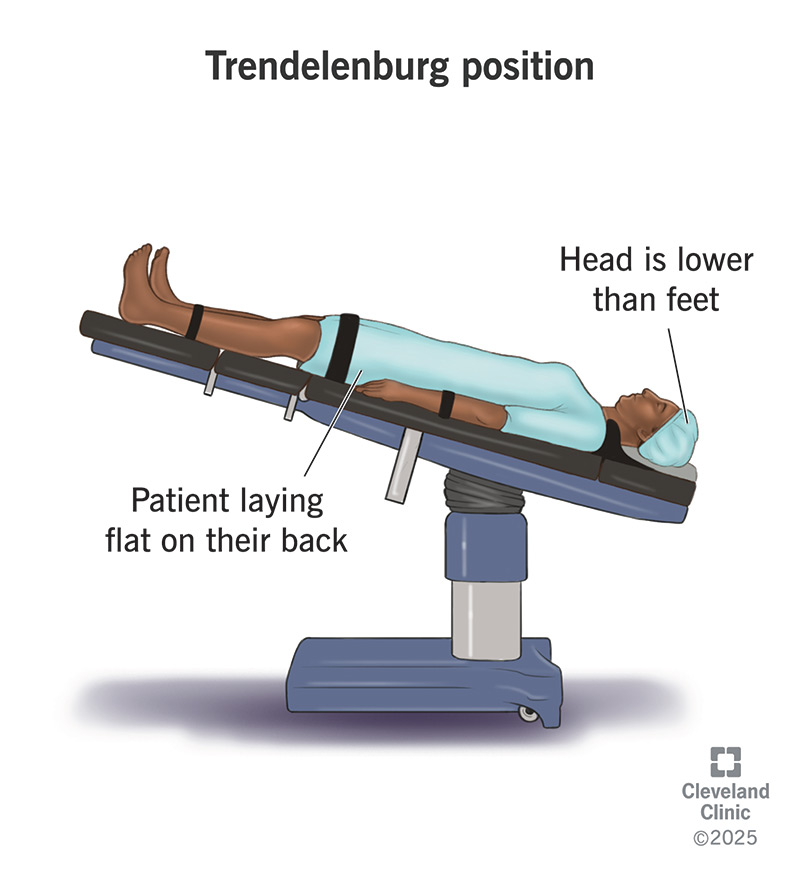
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/trendelenburg-position.jpg)
The Trendelenburg position is a way of positioning you on an operating table or hospital bed for certain medical purposes. A 19th century surgeon named Friedrich Trendelenburg popularized it. Trendelenburg found that positioning a person on their back (supine) and angled slightly downward at the head (at least 15°) makes it easier for a surgeon to access their lower abdominal and pelvic organs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Healthcare providers also use several variations of the Trendelenburg position, including:
The most common uses for the Trendelenburg position are:
There are many organs in your lower abdomen. Your intestines, reproductive organs and urinary system are all smooshed together in there. Other organs sit just above them. Having your feet slightly elevated over your head allows the organs near the top of your abdominal cavity to slide away from the ones near the bottom. This gives your surgeon a little more room to work with those organs.
Advertisement
Another effect of gravity in the Trendelenburg position is that it encourages your blood to flow toward your upper body. This can be helpful for other medical purposes. One common purpose is to place a central venous catheter in your subclavian vein (in your upper chest) or your internal jugular vein (in your neck). Blood flooding into these veins expands them, making them easier to locate and puncture.
Other uses include:
The risks and side effects of the Trendelenburg position relate to the impact of gravity on your upper body. These risks increase with longer procedures, steeper angles and greater body mass. Healthcare providers must pay close attention to these factors when using the position. When appropriate, they use a modified Trendelenburg to reduce the effects. Or they use reverse Trendelenburg to reverse them.
Risks include:
Advertisement
You may be more at risk of complications from the Trendelenburg position if you have:
Healthcare providers weigh these risks against your personal needs when making treatment decisions. Many medical procedures have potential risks, but they also have potential benefits that may outweigh the risks. Care teams take careful precautions to prevent the known risks. In some cases, they might use the Trendelenburg position only briefly, or they might build in regular breaks from it.
If you’re in Trendelenburg position for a longer procedure, your body will need a little time to readjust afterward. You may be swollen with fluid in your face or around your throat. If you had a breathing tube installed for the procedure, your healthcare team will monitor you carefully before removing it. They’ll want to make sure you can breathe normally on your own first.
If you’re only in the Trendelenburg position for a few minutes, you probably won’t need to recover. But if you’re in it for a longer procedure, it may take a few minutes to hours before you feel normal again. You may feel lightheaded or dizzy afterward. If you had surgery, you’re probably also recovering from the effects of anesthesia, which may have similar effects. Try to just take it easy for the rest of the day.
Advertisement
The Trendelenburg position is one of many positions your healthcare team may place you in for medical purposes. Some of these purposes are brief. Others are longer procedures. Any position that’s different from your normal anatomical position can have risks if you’re in it for a long time. It’s your healthcare team’s job to prevent these risks while using the position to enhance your care.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Sometimes you have surgery planned. Other times, it’s an emergency. No matter how you end up in the OR, Cleveland Clinic’s general surgery team is here for you.
