A sleep apnea implant is a surgically implanted device that opens your upper airway as you sleep. It treats symptoms of obstructive sleep apnea. It works by activating the hypoglossal nerve that moves your tongue. It pushes your tongue forward so it’s out of your airway when you breathe.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
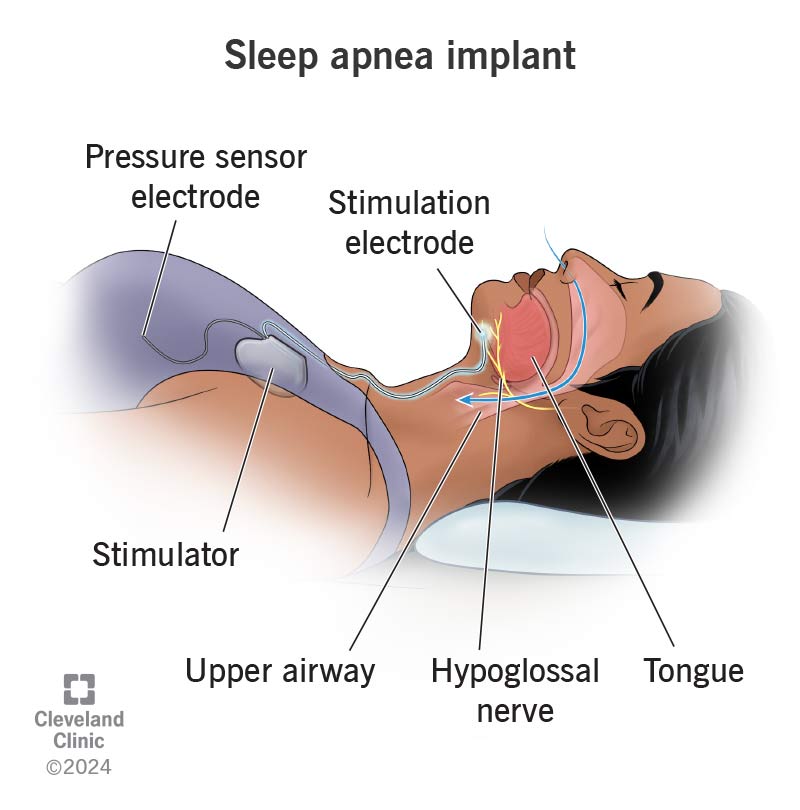
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/sleep-apnea-implant)
A sleep apnea implant is a surgically implanted device that keeps your airway open as you sleep. It helps manage obstructive sleep apnea (OSA) symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Many people choose this procedure if using a continuous positive airway pressure (CPAP) machine isn’t a successful treatment option.
The only current commercially available, U.S. Food and Drug Administration (FDA)-approved implant is the Inspire® upper airway stimulation device. It’s also known as a hypoglossal nerve stimulation device.
The sleep apnea implant activates your hypoglossal nerve. This is the nerve that moves your tongue. If you have obstructive sleep apnea, your tongue may block your upper airway, preventing you from breathing. The sleep apnea device sends an electrical impulse to the nerve. This will move your tongue slightly forward. As a result, your airway stays open as you sleep.
There are four parts to a sleep apnea implant that work together:
Advertisement
You may be a candidate for a sleep apnea implant if you:
A healthcare provider is the best person to talk to if you’re interested in getting a sleep apnea implant. Don’t feel discouraged if you don’t meet one or more of the criteria. There’s a lot for your provider to consider before approving this device as a safe treatment option for you.
Before your provider approves sleep apnea implant surgery, they’ll run a test called a drug-induced sleep endoscopy (DISE) to make sure the device will properly work in your body. You’ll be asleep during the test. Your provider will use an endoscope, which is a device with a small camera on the end of it, to get a closer look at your upper airway, throat and tongue.
Your provider is looking for complete concentric collapse (CCC). This is an upper airway blockage when the sides of your throat and soft palate collapse. CCC may make the device not work.
Your provider will give you specific instructions to follow before the date of your procedure. This may include:
On the day of your procedure, you’ll receive general anesthesia from an anesthesiologist. This will make you sleep for the entire surgery so you won’t feel any pain.
Once in the operating room, your surgeon will:
Your surgeon will place the stimulator device under the skin in your chest, below your collarbone. A very thin wire (pressure sensor electrode) that detects your breathing goes under your ribcage. The thin wire that provides an electrical impulse (stimulation lead electrode) connects to a cuff that wraps around your hypoglossal nerve. This is under your jaw.
Advertisement
It takes approximately 90 minutes to place the implant in your body.
Sleep apnea implant surgery is usually an outpatient procedure. This means that you can go home the same day.
You’ll likely feel sore and slightly swollen after the procedure. Your provider will recommend over-the-counter pain relievers to help you manage this. Symptoms should go away within a couple of weeks as you heal.
Your provider won’t immediately turn on your sleep apnea implant after surgery. They’ll make sure the surgical sites heal as expected before starting treatment. This will take about one month.
You’ll meet with your provider at their office for a follow-up visit after your surgery. During this visit, your provider will examine how well your surgical sites healed and let you know that they’re ready to turn on the device.
The sleep apnea implant works with a remote control — similar to what you’d use to change the channel on your television. Your provider will show you how the remote works. They’ll adjust the settings to stimulate the nerve that moves your tongue. You won’t feel any pain, but you’ll notice your tongue move slightly in your mouth. You can adjust these settings to your own comfort level and under your provider’s guidance.
Advertisement
You’ll use the device every night when you sleep and turn it off in the morning when you wake up.
Your provider will give you instructions on what settings to start using and when you should increase the signal strength. You’ll increase the strength slowly. It usually takes three months to reach the desired signal strength to meet your treatment needs.
When the device is adjusted to an appropriate level, your provider will schedule a sleep study to see how well the device is working. They may recommend changes to the signal strength after the sleep study.
The benefits of a sleep apnea implant include:
As with any type of surgery, a sleep apnea implant comes with possible risks, like:
Once the device is on, you may experience some side effects related to the stimulation, such as:
Your provider may suggest changing the settings on your remote to make the stimulation more comfortable.
Advertisement
You’ll need to rest after surgery for a few days. But you should be able to get back to your regular activities, as long as they aren’t too strenuous. This is usually within a couple of weeks. Your provider will let you know what activities are safe to do during your recovery.
After one month, your provider will show you how to turn on your sleep apnea device and use it. When adjusted appropriately, you’ll undergo a sleep study. Follow-up exams are very important if you get this device. Your care team wants to make sure it works well and it’s helping relieve symptoms of obstructive sleep apnea.
The battery in the implanted device usually lasts around 10 years. A surgeon can replace these batteries by making a small cut (incision) in your skin. They don’t need to remove the entire implant to change the battery. Your provider will monitor battery levels at each follow-up visit.
You may need to change the batteries in your remote more often. You can change these on your own at home.
Let your provider know if you experience severe pain or swelling at the surgical sites, in addition to a fever, after the procedure.
Talk to your provider if you’re having trouble adjusting to the device once you start using it. It may be uncomfortable, but it shouldn’t be painful. Your provider may have some helpful advice, or they’ll make adjustments to the settings so you can manage this.
Wearing a mask at night with a CPAP machine can be uncomfortable or ineffective at managing obstructive sleep apnea symptoms. If this is the case, you and your provider may consider a surgical option like a sleep apnea implant.
While undergoing surgery may be scary, you might be looking forward to getting better sleep once the device turns on. You’ll work closely with your provider to adjust the settings at a pace that’s right for you. It may be awkward at first, but like anything that’s new, you’ll need to give your body time to get used to it. Let your provider know if you have any questions about the implant or your treatment plan following surgery.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Obstructive sleep apnea can keep you from the getting the good night’s rest you need. Cleveland Clinic’s experts can create a treatment plan that helps.
