Responsive neurostimulation (RNS) is a surgically implanted device to treat epilepsy. It detects and responds to abnormal electrical activity at the source in your brain. Similar to a pacemaker, it sends an electrical impulse to a targeted area of your brain to prevent seizures. Studies show it may reduce the number of seizures you have.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
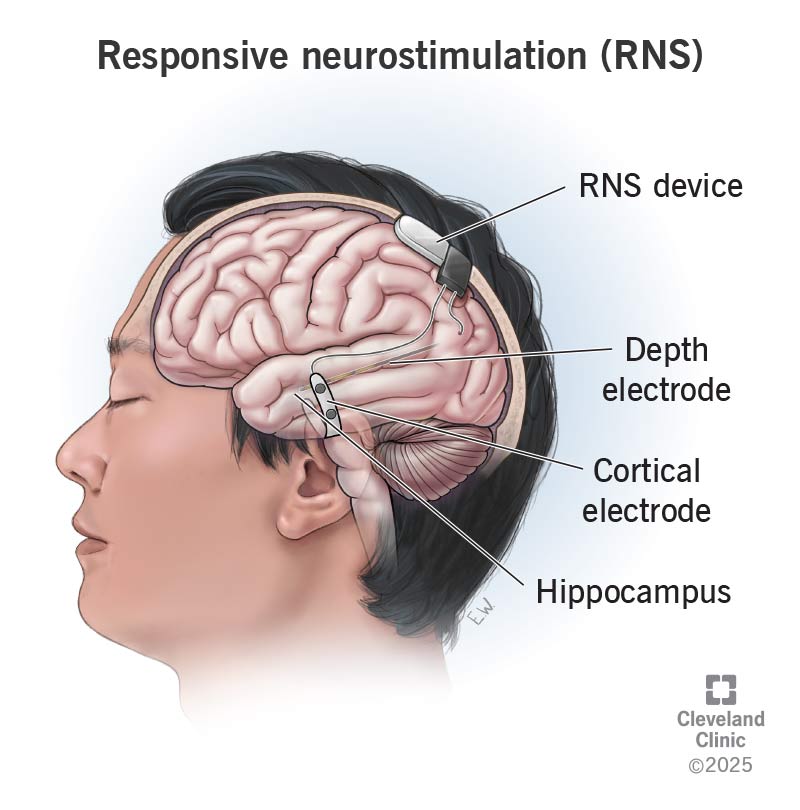
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/responsive-neurostimulation)
Responsive neurostimulation (RNS) is a surgically implanted device that treats seizures. It delivers tiny amounts of electricity to your brain during periods of seizure activity. The RNS® System monitors and detects brain waves in the part of your brain where seizures start. When it notices abnormal electrical activity, it responds very quickly by stimulating that area of your brain with a series of electrical pulses. This electrical energy, over time, decreases your brain’s ability to generate seizures.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A healthcare provider can adjust the RNS System as needed to meet your treatment needs after a surgeon implants the device. A surgeon can also remove it if needed. The RNS System doesn’t cure epilepsy, but it may reduce how many seizures you experience.
RNS may help you manage seizures caused by epilepsy. A healthcare provider may consider this as a treatment option if antiseizure medications aren’t effective. They may also recommend this if other types of epilepsy surgery aren’t possible due to safety concerns or if the outcome of a previous surgery wasn’t successful.
The U.S. Food and Drug Administration (FDA) approved RNS to treat seizures that start in one part of the brain (focal seizures) and don’t respond to other types of treatment. It’s safe for people who are 18 years of age or older.
Your surgeon will make sure you’re healthy enough for the procedure. They’ll perform a physical and a neurological exam, and review your medical history and seizure description history. Let them know if you have any allergies and bring a list of any medications or supplements you regularly take.
You’ll need to undergo testing before the date of your procedure to help your surgeon find the area of your brain where seizures start. This is where they’ll place the RNS electrodes that will help regulate any seizure activity. Your pre-surgery testing may include:
Advertisement
Your provider will also give you instructions specific to your situation. This may include:
On the day of your surgery, an anesthesiologist will put you to sleep using general anesthesia. This is so you won’t feel any pain.
Once you’re in the operating room, your surgeon will:
*These electrodes may be depth electrodes, which your surgeon can place into deep structures of your brain. There’s another type of electrode, called strip or subdural electrodes, which your surgeon will place over the surface of your brain. Your surgeon will decide what type of electrode to use and where it will go before surgery begins.
It usually takes about two to four hours to implant an RNS device.
After surgery, you’ll rest in the hospital. You may need to stay overnight or up to three days in the hospital to make sure you’re healing as expected.
Typically, the device may begin the programming process during your surgery to begin “listening” or detecting potentially abnormal brain signals. The device is usually not programmed to deliver electrical pulses until after you heal from surgery. This could take two to four weeks. You’ll return to your provider’s office, and they’ll turn it on to begin the stimulation treatments.
Your provider will start the electrical stimulation pulses at a low setting. They may increase the settings slowly until they find a level that works well to manage your symptoms. They’ll also fine-tune the detection programming of your device so it better detects your specific abnormal epileptic brain signals.
Advertisement
There’s a lot of information that the device can provide to your physician. The data from the device can be downloaded when you’re home.
The RNS device company will provide you with a computer that has a wand. You place the wand over the device. The computer will download the data and send the data to a secure website called the Patient Data Management System (PDMS). Your physicians will have access to the PDMS data, and they can share details with you, such as how many seizures the device recorded and what time of day these seizures are occurring.
Physicians can use this data to make other decisions, like changing a medication dose during times when epileptic activity is more frequent. Your physician will also download data during your follow-up visits. They can show you and explain what the data looks like.
The benefits of an RNS device may include:
The RNS System has a good success rate. Many people report fewer seizures in the years following surgery. In a nine-year study, the typical patient had about a 75% reduction in the amount of seizures over nine years of treatment. This means that if you had about 10 seizures per month prior to starting RNS, then you may be down to three seizures a month after nine years of treatment. There were 18% of study patients who were seizure-free for more than one year during the study.
Advertisement
RNS surgery comes with possible risks. While rare, these may include:
There are typically no persistent side effects from electrical stimulation, as the stimulation is tested in the office with your physician to ensure that you’re tolerating it well.
Contact your healthcare provider if you notice symptoms after surgery like severe pain, bleeding or swelling at the incision site.
Once your provider turns on the RNS device, let them know if you experience any symptoms that are uncomfortable like feeling lightheaded, vision changes or numbness. The RNS System is adjustable, so your provider can make changes to the amount of stimulation you receive if it’s unpleasant.
You should be able to return to your daily routine when you leave the hospital. Be careful not to overwork yourself and don’t participate in strenuous activities unless your provider approves it. You may return to work or school in two to four weeks. Your provider will make sure you’re healing as expected during follow-up visits. It could take up to eight weeks to make a complete recovery.
The average RNS device battery, from the most recent device, can last up to eight to 10 years. The battery life varies based on frequency of use and type of battery. Your provider will let you know what you can expect.
Advertisement
To replace the battery, you don’t need to replace the entire device. A surgeon can perform a smaller procedure where they open the previous incision site, replace the battery and then, close the incision while leaving the original electrodes in place.
You might be feeling a lot of emotions as your provider prepares you for surgery. It’s normal to be nervous and scared. It’s also normal to feel excited as you anticipate the outcome.
Your care team will walk you through what you can expect to put you at ease. This includes pre-surgery testing to find the area of your brain that’s causing seizures, your recovery and follow-up visits, and programming the device.
Don’t hesitate to contact your provider if you have any questions or concerns about the procedure or the RNS device. They’ll have up-to-date information on the device’s anticipated battery life and any additional care tips you should keep in mind.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Epilepsy and seizures can impact your life in challenging ways. Cleveland Clinic experts can help you manage them and find relief.
