A colostomy is a surgical procedure that changes the way stool (poop) exits your body. When medical reasons require you to bypass part of your colon, surgeons make a new opening in your abdominal wall for poop to come out. The poop collects in an attached pouch (colostomy bag). The operation can be temporary or permanent.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
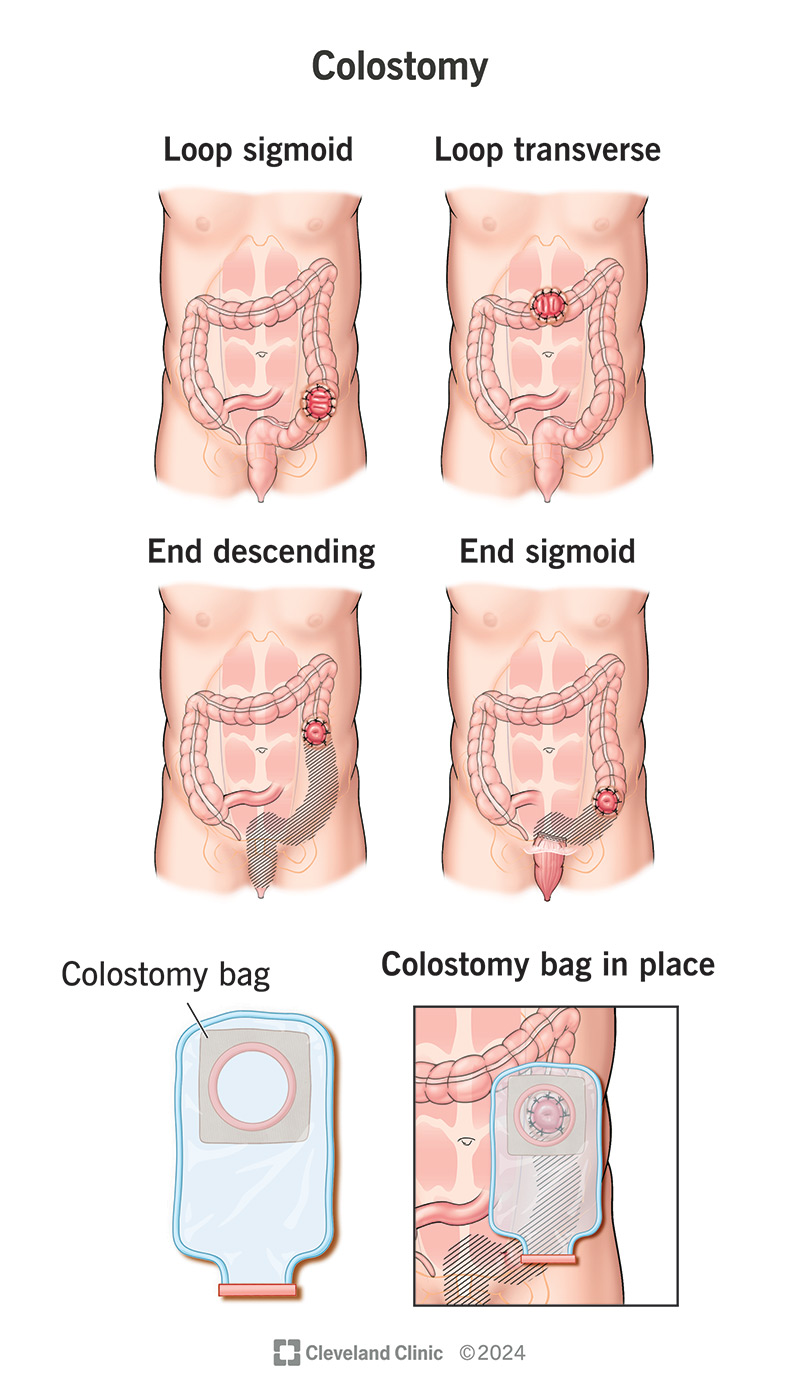
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/22100-colostomy.jpg)
A colostomy is a surgery that changes the way stool (poop) exits your body. During the procedure, a surgeon creates a hole (stoma) in your abdominal (belly) wall. They then connect a portion of your colon to it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Instead of pooping like you used to, waste collects in a pouch (or colostomy bag) on the outside of your belly. Some people only have a colostomy for a few months, while others need one for life.
A colostomy is a type of ostomy. It may be part of a colectomy operation, a procedure to remove part or all of your colon. Other conditions may require you to stop using your colon, either temporarily or permanently. After surgery, “colostomy” also refers to your newly redirected colon. Your healthcare provider will talk to you about living with and caring for your colostomy.
There are several types of colostomies. The names of these procedures correspond with the portion of your colon that a healthcare provider must redirect.
Advertisement
Your healthcare provider will consider many factors. This helps them choose the best option for your situation. Most importantly, it depends on whether you need a temporary or permanent solution.
You may need a colostomy if a health condition keeps you from using your colon or anus like you used to. It might be a temporary intervention that allows your body to heal or it may be a permanent solution for an irreversible condition.
Some conditions that may require a temporary colostomy include:
Some conditions that may require a permanent colostomy include:
A colostomy is a major surgery, and it involves some preparation.
You’ll have a pre-op assessment with your surgeon. Before you sign your consent forms, they’ll make sure you understand the procedure, the risks involved and the lifestyle changes you’ll have to make afterward. You may also discuss your pain management options at this time.
They’ll also take a blood sample to check that you are well enough for surgery. They may also run an EKG test to check that your heart is in good health.
Another healthcare provider (usually a nurse) will teach you about your future ostomy. They’ll also help you choose the best location for the colostomy on your abdomen.
You’ll need to avoid eating for six hours before surgery and drinking clear liquids two hours before surgery. Your surgeon might also recommend an enema or bowel prep (like before a colonoscopy) to take at home.
You’ll be under general anesthesia for your colostomy. Depending on your situation, your surgeon may do open surgery or laparoscopic surgery.
Open surgery requires a longer incision across your abdomen. Laparoscopic surgery is less invasive. Instead of making one long incision, your surgeon will make several small incisions. Then, they’ll put a tiny camera and special instruments through the incisions. They’ll use these to perform the surgery inside your belly.
During your colostomy operation, your surgeon creates an opening (stoma) in your abdominal wall. Then, they attach part of your colon to your new stoma. For a sigmoid or descending colostomy, your stoma will be on the lower left side of your belly. If you have a transverse colostomy, your stoma will be somewhere across your upper belly, or on the right or left side.
Advertisement
Once your surgeon completes your colostomy, they’ll attach a colostomy bag to your skin. There are several types of colostomy bags. They include closed bags, drainable bags and mini pouches. Your healthcare provider will help you choose the best option for your needs.
You’ll need to recover in the hospital for the next three to seven days. During this time, you’ll:
A colostomy is often a life-saving intervention. If you need a colectomy or similar operation, a colostomy lets your body keep working after losing a major organ.
Colostomy can also give your colon a “time out” after a procedure. Or you might need to rest your colon following illness or injury. Colostomy allows healing to take place safely without risking further complications.
Advertisement
Colostomy is a common and straightforward surgery. It’s generally safe, but there are always some risks, including:
Even after a successful colostomy, you might develop complications down the road. These may include:
Advertisement
Each person heals at a different pace. But on average, most people recover from colostomy surgery within six to eight weeks.
Be sure to follow your surgeon’s post-op guidelines. It’s important to get lots of rest. But you should also take short walks around your house. Short walks help your bowels move more quickly.
Contact your healthcare provider if you experience:
Pooping will be different with a colostomy bag. After your surgery, your anus may continue to expel small amounts of poop and other fluids that remain inside (even weeks to months after surgery). But new poop will now exit through your stoma. Most people will be able to feel their bowels move and know when poop is about to come out. But you won’t be able to control it anymore. Unlike your anus, your stoma doesn’t have a muscle system that allows you to close it at will. So, pooping won’t be the intentional action that it used to be.
After colon removal, some people may continue feeling phantom bowel movement urges. These urges are similar to phantom limb syndrome. They find that the urges subside if they sit on the toilet like they used to. If you still have your anus intact and you don’t have a separate stoma for anal discharge, you’ll continue to pass occasional mucus through your anus. This will feel similar to a bowel movement. The inactive colon continues to produce mucus as it always did, to lubricate and protect the skin.
Waste should begin passing through your stoma about three to seven days after your colostomy.
Many people always wear their colostomy bag to catch poop when it comes out. Modern colostomy bags are discreet, and you can wear them under almost any kind of clothing. People who have had descending or sigmoid colostomies may be able to predict when they need to poop. They only wear a pouch during those times. They also may be able to induce pooping through colostomy irrigation. By spending time daily clearing out their bowels with water, people can go without a bag between irrigations.
This will depend on a few factors, including:
You can discuss plans for a reversal with your provider during your follow-up visits. They’ll assess your condition and schedule your reversal surgery when they feel you’re ready. It might be a few months to a year after your first surgery. Sometimes, it’s several years. There’s no time limit to a reversal, only health limits.
A colostomy is a life-changing — and often, life-saving — operation. Whether you need a temporary or permanent solution, life with a colostomy requires a substantial adjustment. But you’re not alone. There’s a wide community of people living with ostomies who can help initiate you and offer companionship throughout your journey. There are also numerous products available to make life with colostomy easier. People with colostomies can live full and normal lives, and often enjoy more comfort and freedom than they did before the operation.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Some conditions like rectal and colon cancer, Crohn’s disease and ulcerative colitis may require colorectal surgery. Cleveland Clinic has the expert care you need.
