Psoas syndrome can cause pain in your hips, lower back, butt or groin. It might be hard to tell what’s causing it because there are so many muscles in those areas of your body. Visit a healthcare provider if you’re in pain for more than a week, especially if it hurts to move or use your hips.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
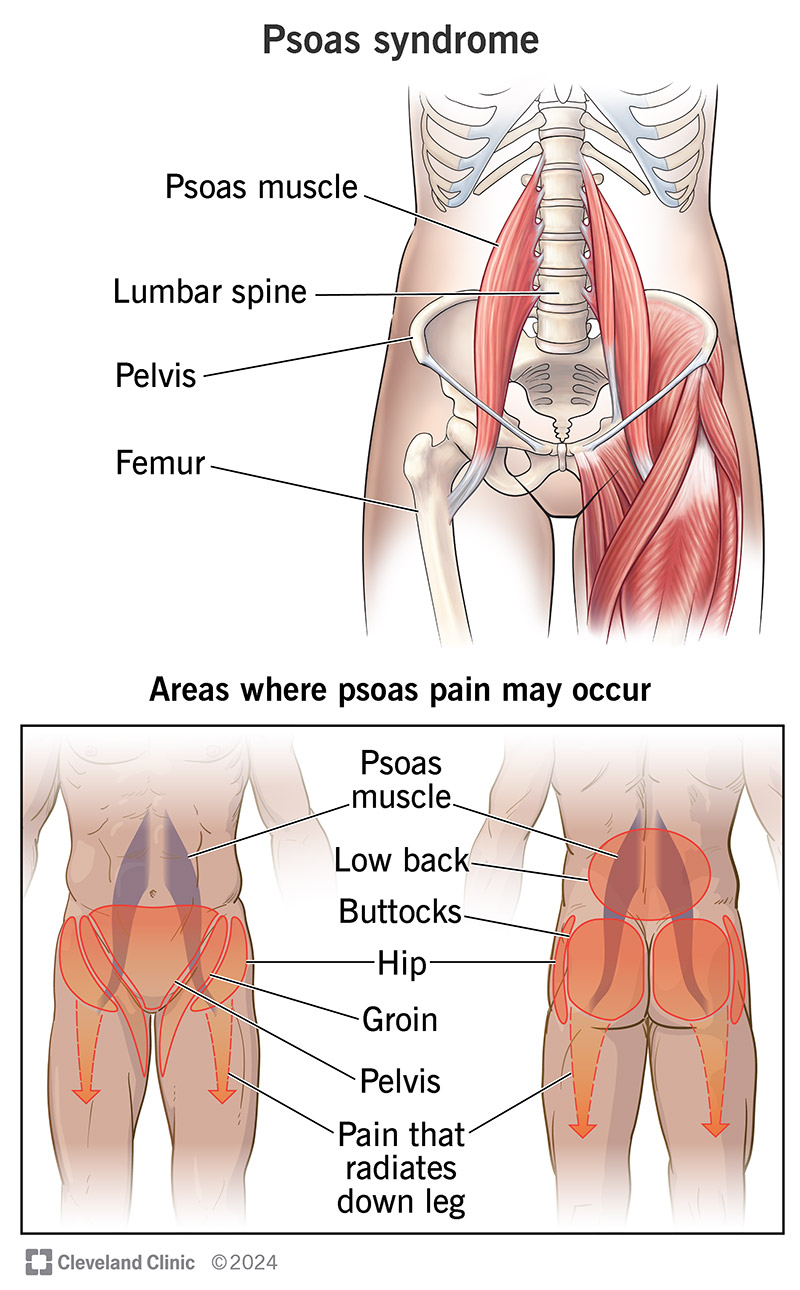
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/psoas-syndrome)
Psoas syndrome is painful irritation or an injury in one of your psoas muscles. Healthcare providers sometimes call psoas syndrome iliopsoas syndrome. Psoas is pronounced SO-ezz.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The psoae (the plural form of psoas) are a pair of long muscles that run from your lower back to the top of your hips on either side of your spine.
Psoas syndrome causes pain in your lower back, hips or groin. Visit a healthcare provider if you’re experiencing pain that doesn’t get better in a week.
Psoas syndrome is rare. Many people who have it never get it diagnosed because symptoms usually get better before they visit a healthcare provider.
Experts think psoas syndrome is often misdiagnosed or underdiagnosed because it shares so many symptoms with other injuries or health conditions. The good news is that, in most cases, the same treatments that manage other, similar issues also treat psoas syndrome.
Psoas pain is the most common psoas syndrome symptom. You might feel:
Psoas syndrome pain may get worse in certain positions or during physical activities. The pain might spread (radiate) down your legs or get worse when you try to stand up straight. You might notice pain that’s bad enough to make you limp or shuffle your feet when you walk.
Advertisement
Overusing your hips and sports injuries are the most common causes of psoas syndrome.
Some cases of psoas syndrome happen without an obvious cause (idiopathic psoas syndrome).
Rarely, psoas syndrome happens when infections or cancers spread to your psoae.
Anyone can develop psoas syndrome, but athletes are the most likely to have it. Sports that put a lot of repeated stress on your hips can increase your risk, including:
Teens and children who play sports may have a higher risk because their bodies are changing and developing quickly, which can make their muscles more susceptible to injuries or irritation.
People who’ve had recent hip surgeries (especially hip replacement) may experience psoas syndrome as a temporary side effect.
Psoas syndrome doesn’t usually cause complications. Severe cases may make it painful or difficult for you to stand, walk or move, but these symptoms usually get better when you start treatment.
A healthcare provider will diagnose psoas syndrome with a physical exam. They might also use some imaging tests.
Your provider will examine your hips, legs and spine. They might ask you to move or sit in different positions. Tell your provider when you first noticed pain or other symptoms, and if certain activities or times of day make the symptoms worse (or better).
Diagnosing psoas syndrome is usually a differential diagnosis. This means your provider will rule out other, more common injuries or conditions that might cause similar symptoms before diagnosing psoas syndrome.
Some musculoskeletal issues that cause similar symptoms include:
Health conditions that aren’t injuries can also share symptoms with psoas syndrome, including:
Your provider might use a few different types of imaging tests to take pictures of your spine, hips and the areas around them, including:
A healthcare provider will suggest treatments for psoas syndrome depending on what caused it. The most common treatments include:
Psoas stretches are specific stretches or posture changes that target the psoas. People also sometimes call them psoas releases.
Advertisement
Even though you can do these stretches safely at home, make sure you talk to a healthcare provider or physical therapist before starting any new exercise routine, especially if you think you have a specific injury like psoas syndrome. They’ll tell you the best stretches for your specific needs and show you how to perform them safely. Never try to self-diagnose a health condition or injury.
Your physical therapist might prescribe a core stabilization program. These are exercises designed to strengthen your core muscles and improve how well you can move your core between your spine and pelvis.
Psoas syndrome usually goes away with treatment and exercises. You should be able to regain a full range of motion (how far you can move parts of your body) and resume your usual level of physical activities.
It usually takes a month or two to recover from psoas syndrome. The pain should start getting better gradually after you start physical therapy or OMT. Your provider will tell you when it’s safe to resume training or intense physical activities.
Stretching and warming up before exercise or physical activity are the best ways to prevent all types of muscle injuries. Increasing your overall flexibility will also protect your muscles from injuries. Your physical therapist can help you modify (change) your posture when you’re sitting, exercising or doing other physical activities to prevent irritating your psoae.
Advertisement
Increase your activity level gradually. Don’t suddenly ramp up your training intensity or start exercising way more often than you usually do. Some people with psoas syndrome need to temporarily change how they exercise. You might need to stick to shallower weightlifting positions or exercise ranges, for example. Some people need to avoid running on inclines (hills).
Visit a healthcare provider if you feel pain, stiffness or other symptoms that don’t get better after a week of rest. Talk to your provider or physical therapist if it feels like your physical therapy or exercises aren’t managing your symptoms — or if you feel like the pain is getting worse or changing.
You may want to ask your provider:
Psoas syndrome is a rare pain in the butt, sometimes literally. It happens when the psoas muscles on either side that extend from the bottom of your ribs to the top of your hips are injured or irritated. This can cause pain in your lower back, hips, groin or butt.
It can be annoying to have to change how you exercise or do other physical activities. Especially if you have to take a break and avoid them entirely for a while. But it’s worth the wait. You should be able to resume all your usual workouts and routines once your psoae heal.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Are you recovering from an injury, surgery or illness? Cleveland Clinic’s physical therapy team will help you get back to what you love to do.
