Trichophyton mentagrophytes genotype VII (TMVII) is a sexually transmitted fungal infection. That means it mainly spreads through anal, vaginal or oral sex. It causes rashes around your penis or vulva, butt, face or legs. The rash can be itchy or painful. Providers treat it with antifungal medications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
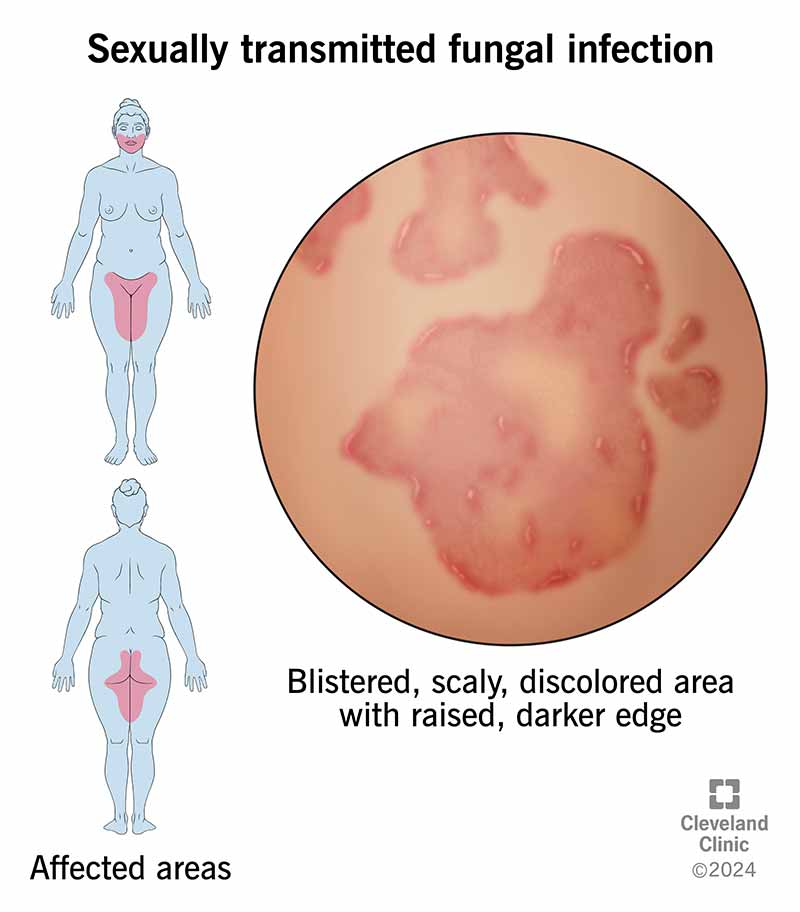
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/sexually-transmitted-fungal-infections.jpg)
A sexually transmitted fungal infection is a skin rash that spreads mainly through oral, anal or vaginal sex. The fungus Trichophyton mentagrophytes type VII (TMVII) causes it. It forms itchy, painful patches of skin around your penis or vulva (genitals), butt, face or legs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
TMVII is the only known sexually transmitted fungal infection. Other fungal infections, like jock itch and yeast infections, can sometimes spread through sex, but they’re not considered sexually transmitted infections (STIs). The rash caused by TMVII is often more severe than other kinds of fungal infections in your skin.
Trichophyton mentagrophytes infections around your genitals are also called tinea genitalis.
The main symptom of sexually transmitted fungal infections is a rash. The rash might be:
The fungus Trichophyton mentagrophytes genotype VII (TMVII) causes sexually transmitted fungal infections. It’s a type of ringworm.
TMVII spreads between people by touching the rash. It can spread through sex or by sharing personal items, like towels or sex toys.
Anyone who’s been in contact with TMVII can get infected. But men who have sex with men and people who exchange sex for money are at a higher risk.
TMVII can sometimes lead to secondary bacterial infections (bacterial infections that happen at the same site as the fungal infection) that require treatment at a hospital. The rash can also cause scarring.
Advertisement
Your provider might think you have a fungal infection based on the appearance of the rash. If it doesn’t go away with topical antifungals (creams or lotions), they may suspect it’s TMVII (topical antifungals don’t work on TMVII).
A provider diagnoses TMVII by scraping a sample of skin from the rash and testing it. A lab will look for Trichophyton mentagrophytes under a microscope. They might try to grow (culture) fungi from the sample. These tests can sometimes take a few weeks, so your provider may start treatment before the results are back.
Treatment for TMVII is antifungal medications you take by mouth, like terbinafine or itraconazole. Antifungal creams or lotions don’t work on TMVII fungal infections.
If you have a sexually transmitted fungal infection, it might take a while to feel better. You’ll have to take antifungal medication for anywhere from two weeks to a few months. During this time:
You can reduce your risk of getting and spreading sexually transmitted fungal infections by:
Contact your provider if you have a persistent or painful rash. If a provider has prescribed an antifungal cream or lotion and the rash hasn’t gone away, let your provider know.
Go to the emergency room if you have a high fever (over 103 degrees Fahrenheit/40 degrees Celsius) or a rash or wound that is:
It might be helpful to ask your provider:
Sexually transmitted fungal infections aren’t as simple to treat as other fungal rashes, like jock itch. A cream won’t make TMVII go away — but it can be cured with prescription antifungal medications. You’ll have to take them for several weeks to feel better. Don’t hesitate to ask your healthcare provider if you have any questions or concerns.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Don’t ignore sexually transmitted infections. Cleveland Clinic experts will treat them confidentially and quickly in a judgment-free environment.
