Genital herpes is a common infection that causes sores or blisters on your genitals. The herpes simplex virus (HSV-1 and HSV-2) causes it. Although there isn’t a cure for herpes, there are ways to prevent its spread and treat outbreaks. Safe sex practices are key to preventing genital herpes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
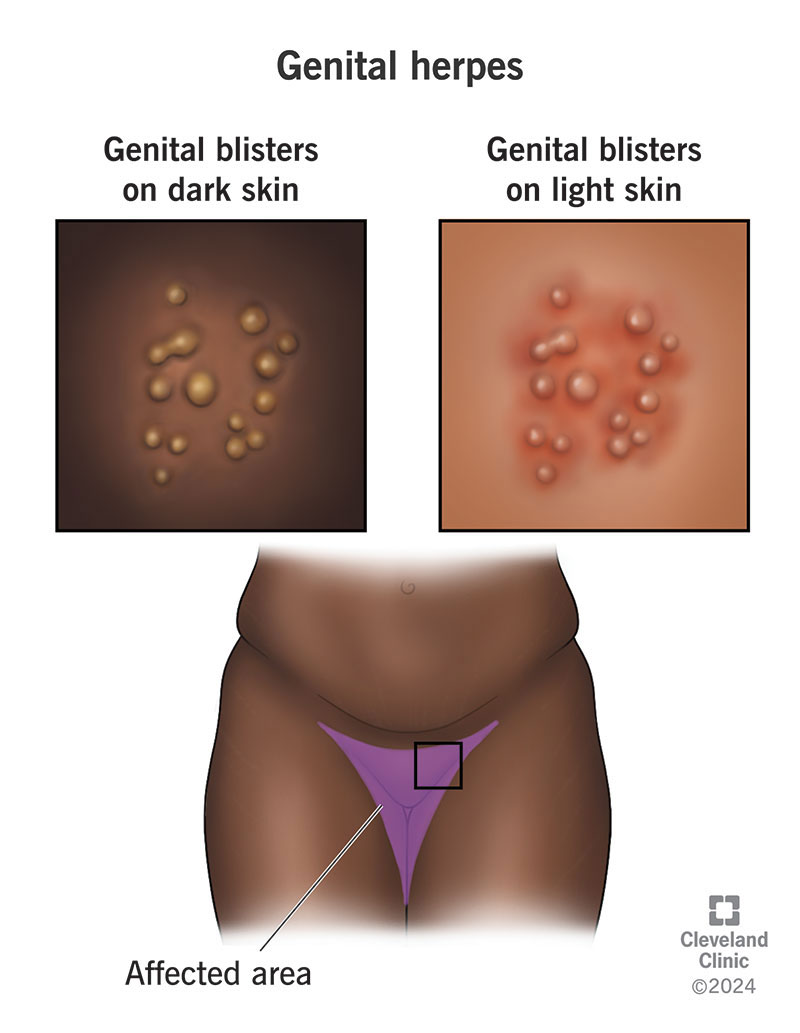
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/genital-herpes)
Genital herpes is a contagious sexually transmitted infection (STI) that causes you to develop painful blisters (or sores) on your genitals. The sores can affect your:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The herpes simplex virus (HSV) causes genital herpes. There are two types of HSV: HSV-1 and HSV-2. Both types can give you genital herpes, although HSV-2 causes it much more frequently.
Genital herpes mainly spreads through vaginal, oral and anal sex. But you can also get genital herpes from someone with oral herpes. Oral herpes can spread from the mouth to the genitals and become genital herpes.
There’s no cure for genital herpes. Once you have the virus in your body, it stays in your body for the rest of your life. Taking medication can help your symptoms and lower the risk of spreading the infection. Using a condom, taking medication and avoiding sexual intercourse when you have a genital herpes outbreak can prevent you from giving it to your partner.
The Centers for Disease Control (CDC) estimates that up to 50 million people in the U.S. have genital herpes. Estimates show almost 600,000 people are newly infected each year in the U.S.
Globally, about 491 million people between ages 15 and 49 have HSV-2, the most common cause of genital herpes.
Advertisement
Symptoms vary and depend on if it’s your first outbreak or a recurrent outbreak. Recurring symptoms are usually milder than the first outbreak. Symptoms also don’t last as long with later outbreaks. Some people may only have one or two outbreaks during their lifetime. Others may have as many as four or five outbreaks a year.
When symptoms occur, they’re usually worse during the first outbreak. Symptoms typically appear within two to 20 days after infection. Your symptoms may last up to four weeks.
You may experience:
Recurrent outbreaks or flare-ups happen any time after the first outbreak (even if it’s years later). You can’t control when a recurrent outbreak occurs or how often it occurs. But your symptoms are usually less severe, and the outbreak is generally milder and shorter.
Genital herpes typically begins as small, blister-like bumps. They tend to appear in a cluster. You may feel itchiness or tingling in the area 24 to 48 hour before a sore appears. The blister will take on a sore or ulcer-like appearance, then eventually open and ooze. Then, a scab will appear as the ulcer heals. Once the ulcers fully heal, the scabs fall off and that outbreak is complete.
Genital herpes is a sexually transmitted infection or STI, also called a sexually transmitted disease or STD. The two types of herpes simplex virus (HSV-1 and HSV-2) cause genital herpes. HSV-2 is the most common cause of genital herpes.
The herpes virus that causes genital herpes spreads through saliva, semen and vaginal secretions. It’s possible to get genital herpes from someone who doesn’t have visible symptoms. You can have the infection, not know it and infect someone else.
Genital herpes can spread through:
You can’t get genital herpes from objects like toilet seats. It’s not likely that you’ll get genital herpes from surfaces like towels or clothing, either. But you could pass genital herpes through shared sex toys. To stay safe, wash sex toys before and after using them, and don’t share them. If you do, protect them with a condom.
Genital herpes is highly contagious. You’re most contagious when you have an open sore. Even if you don’t have open sores or symptoms of an outbreak, it’s still possible to infect another person with the herpes virus. This is called asymptomatic shedding.
Advertisement
Yes. Both HSV-1 and HSV-2 can infect your mouth and your genitals. You can get herpes sores on your genitals if you receive oral sex from someone who has a cold sore from HSV-1.
There isn’t a cure for HSV-1 and HSV-2, the virus that causes genital herpes. Because the virus lives dormant (or inactive) in your body, you can get a genital herpes outbreak again (called a recurrence or flare-up). There’s no rhyme or reason as to why some people get more outbreaks and others get fewer. But healthcare providers know that certain activities tend to reactivate the virus. These include:
Some people never develop symptoms. They don’t know they have the virus that causes genital herpes. They may unknowingly infect others. You can have the herpes virus for years and not have symptoms, so it’s hard to know when or from whom you got it.
Yes. If your partner has genital herpes and takes precautions not to spread it to you (like wearing condoms and taking medication), it’s possible that you won’t get it.
Genital herpes affects anyone who’s sexually active and not taking precautions to prevent the spread of STIs. Your risk may be higher if you:
Advertisement
Complications from genital herpes include:
If you’re immunocompromised, you may experience more severe outbreaks. Rarely, genital herpes can cause infections in your brain (encephalitis) or the membranes around your brain and spinal cord (meningitis).
Genital herpes doesn’t affect fertility or your ability to conceive. If you're pregnant and have genital herpes, you should start a daily antiviral at 36 weeks of pregnancy to prevent outbreaks during delivery. If you have an active infection at the time of childbirth, you can pass the herpes virus to your baby. Your healthcare provider will perform a C-section to lower this risk.
Advertisement
Yes, as long as there isn’t an open lesion on your chest or breast, you can breastfeed. If you have an active outbreak while breastfeeding, it’s possible to spread the infection to your nipples through touch. Careful handwashing can prevent this spread. You shouldn’t nurse from a breast that has herpes sores. You can pump breast milk until the sores heal. Don’t give your baby expressed breast milk if the pump comes into contact with an open sore.
In addition to a physical exam, your healthcare provider will take a fluid sample from an open sore to test for the herpes virus. If your blisters have healed or you don’t have blisters, a blood test can check for HSV-1 and HSV-2 antibodies, a marker showing you have the virus in your bloodstream.
The blood test doesn’t show an active infection (especially in the absence of open sores or lesions). But it informs your provider that you’ve been exposed to the herpes virus in the past. If this is your first infection, you likely won’t test positive for herpes because there hasn’t been enough time for your body to develop antibodies.
Your healthcare provider will likely recommend you have a blood test to check for other STIs (syphilis, gonorrhea, chlamydia).
There isn’t a cure for genital herpes. But there are ways to treat active genital herpes outbreaks and manage the symptoms it causes. You should avoid sexual contact until genital herpes sores have completely healed.
Your healthcare provider may prescribe antiviral medications like valacyclovir (Valtrex®) or acyclovir (Zovirax®) to help manage symptoms of genital herpes. These medications can:
The benefits vary according to how often you take the medication. Treating a single outbreak doesn't have any effect on the severity or frequency of future outbreaks. But your provider may prescribe chronic suppressive therapy (taking medication every day) to help you have less severe and less frequent outbreaks in the future.
If you have mild symptoms or infrequent outbreaks, you might not need or want treatment.
During an outbreak, these steps can ease your symptoms:
Wash your hands after contact with any genital herpes sore. Try not to touch the sores, as this just increases the risk of spreading it to other parts of your body.
It depends on if it’s your first outbreak or a recurring outbreak. Your first outbreak tends to last longer than recurrent outbreaks. You can expect to have symptoms of a first outbreak for up to four weeks. In subsequent outbreaks, your symptoms may go away after two weeks.
Keep in mind that genital herpes doesn’t ever go away. You may not have visible sores or blisters, but you’ll always have HSV, the virus that causes genital herpes.
No. Once you have HSV, the virus that causes genital herpes, you have it for life.
Many people who find out they have herpes feel embarrassed or ashamed knowing they’ll always have the virus and can give it to others. But you aren’t alone. Herpes is one of the most common STIs, both in the U.S. and worldwide. If you have herpes, you should:
If you have herpes, you can still:
Your first outbreak may last up to four weeks. Recurrent outbreaks usually last between one to two weeks.
If you’re sexually active, you can take these steps to protect yourself and others from the herpes virus and other STIs:
If your sexual partner has genital herpes, these actions can lower your risk of getting the virus:
You should call your healthcare provider if you experience:
You may want to ask your healthcare provider:
Hundreds of millions of people are living with genital herpes (and some may not even know!) around the world. Still, it’s normal to feel shame or embarrassment about a diagnosis, especially when you have to discuss the virus with your healthcare provider or your sexual partners. But don’t let your emotions hold you back from having honest conversations or seeking medical care. Treatment with antiviral medication can ease your symptoms, reduce outbreaks and protect sexual partners from infection. Having genital herpes shouldn’t affect your relationships or sexual health. But you should tell your partners that you have it. Wearing condoms, taking antivirals and avoiding sex when you have an active outbreak are the best ways to lower the risk of spreading genital herpes to your partners.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Have a virus, fungus or bacteria? Some of these “bugs” won’t go away on their own. Cleveland Clinic’s infectious disease experts are here to help.
