Bronchiolitis is a viral infection that targets the small airways of a child’s lungs. It causes wheezing, coughing and a slight fever. It’s most common during colder months. Contact your child’s healthcare provider or emergency services if your child has trouble breathing.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
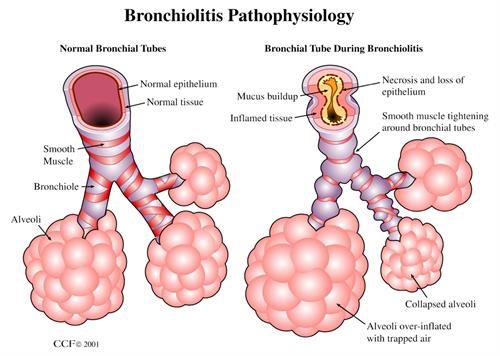
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/8272-pediatric-bronchiolitis.ashx)
Bronchiolitis is a viral infection that affects children younger than 2 years old. It causes the airways (bronchioles) in your child’s lungs to narrow, which makes breathing difficult. If your child develops this infection, you may notice they have symptoms similar to a common cold (runny nose, cough) in addition to noisy breathing (wheezing).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The infection is seasonal. It’s more likely to occur during the winter and early spring.
Bronchiolitis isn’t usually serious, but it can be. If your child develops this infection, monitor their breathing and contact a healthcare provider if they have trouble breathing.
Bronchiolitis is the most common lower respiratory tract infection among children younger than 2 years old.
The viruses that cause bronchiolitis are contagious. These viruses spread through respiratory droplets (saliva or mucus) from someone’s mouth or nose. When someone sneezes or coughs, these droplets become airborne and spread from person to person or stick to frequently touched surfaces or objects.
Bronchiolitis and bronchitis are two conditions that both sound similar and have similar symptoms. A virus causes both conditions, which target the airways in your lungs. Bronchitis affects the bronchi, or the larger airways. Bronchiolitis affects your smaller airways (bronchioles). Bronchitis usually affects older children and adults, while bronchiolitis is more common in younger children.
Early signs and symptoms of bronchiolitis resemble those of the common cold, including:
Advertisement
A bronchiolitis infection targets your child’s airways and can cause the following symptoms that affect their breathing:
If your child has trouble breathing or you notice the following symptoms of severe bronchiolitis, call their healthcare provider or visit the emergency room immediately:
A virus causes a bronchiolitis infection. Viruses that can lead to bronchiolitis include:
Bronchiolitis most often affects children younger than 2 years old. Adults can get bronchiolitis, but it’s rare. Your child may be more at risk of developing severe bronchiolitis if they:
Complications of bronchiolitis include:
Bronchiolitis can be life-threatening if your child has severe symptoms that affect their ability to breathe. If you notice your child has difficulty breathing, contact 911 or local emergency services or visit the emergency room immediately.
Your child’s healthcare provider will diagnose bronchiolitis after a physical exam and testing. During the exam, your child’s provider will check their vital signs and temperature and listen to their breathing through a stethoscope (auscultation).
You can expect your child’s provider to ask you questions about their symptoms, like:
Your child’s provider may place a pulse oximeter (pulse ox) on their fingertip or toe to determine how much oxygen is in their blood (blood oxygen level).
Testing might include a nasal fluid culture, which is a swab that collects fluid from the inside of your child’s nose to detect viruses. If your child has severe symptoms, a chest X-ray might be necessary.
Advertisement
Bronchiolitis has symptoms that are similar to other respiratory infections like bronchitis and pneumonia. It may seem like asthma, which can cause wheezing and trouble breathing. You might wonder if your child breathed in (aspirated) something other than air.
Any time that you notice that your child has problems breathing, you should call their healthcare provider. They’ll be able to diagnose one breathing issue from another.
Treatment for bronchiolitis focuses on symptom relief, including:
Bronchiolitis doesn’t always need treatment, so talk to your child’s provider if they have symptoms. Antibiotics won’t help because they’re ineffective at treating viral infections.
Your child may need to stay in the hospital if they have trouble breathing. Your child may need oxygen therapy or intravenous (IV) fluids in the hospital.
In addition to monitoring your child’s breathing during their illness, you can help your child feel better at home by:
Advertisement
Most children diagnosed with bronchiolitis feel better within one week. Their breathing may improve after a few days, and most symptoms should clear up after about a week. Rarely, mild symptoms may persist for another week or two. Your child may cough for up to a month.
Your child may have symptoms for up to a week if they have bronchiolitis. During their illness, they may have trouble eating full meals or lose their appetite. To help your child eat when they don’t want to, try feeding them multiple small meals throughout the day instead of larger meals less often. It’s important to keep your child hydrated since they’re at a high risk of dehydration during their illness.
To alleviate your child’s symptoms, talk to their healthcare provider to see what’s safe for your child to take, like over-the-counter (OTC) medications to reduce a fever. Don’t give your child aspirin, as it can lead to Reye’s syndrome.
If your child has symptoms that don’t improve after one week or get worse, contact their healthcare provider. If your child has trouble breathing, contact emergency services or visit the emergency room immediately.
Some children develop asthma as they grow if they had bronchiolitis when they were infants. While less common, some children may develop pneumonia after bronchiolitis.
Advertisement
Yes. Since there are many viruses that can cause bronchiolitis, your child can develop the infection more than once.
It’s difficult to prevent bronchiolitis since the viruses that cause it are common. You can take steps to lower your child’s risk of developing bronchiolitis by:
Until your child is better, keep them home from daycare or other environments where they’re in close contact with others. The virus that caused their illness is contagious.
Call your child’s healthcare provider if your child:
Don’t be afraid to call a healthcare provider if your child doesn’t seem to be getting better or if you’re worried about something.
Call 911, your local emergency services number or take your child to the emergency room if they have trouble breathing. A sign of this is when your child’s nostrils flare or their chest retracts when they try to breathe.
Questions to ask your child’s healthcare provider include:
Bronchiolitis affects your child’s airways. This can make breathing difficult for them. You may first notice your child has symptoms of a cold along with noisy breathing. If you’re worried about your child’s breathing, contact their provider. Treatment is available to relieve your child’s symptoms and help them feel better. While the infection clears up, it’s normal for your child to cough for a few weeks following their illness. If your child has symptoms that get worse instead of better, call their provider.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Need care fast? Cleveland Clinic’s Express Care and Urgent Care locations treat everything from sprains to sinus infections — no appointment needed.
