Balanitis is a treatable condition that most commonly happens in uncircumcised males. The main symptoms of balanitis include inflammation and pain on the head of your penis. Treatment often includes antifungal creams, antibiotics, regularly cleaning the area and, in some cases, circumcision.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
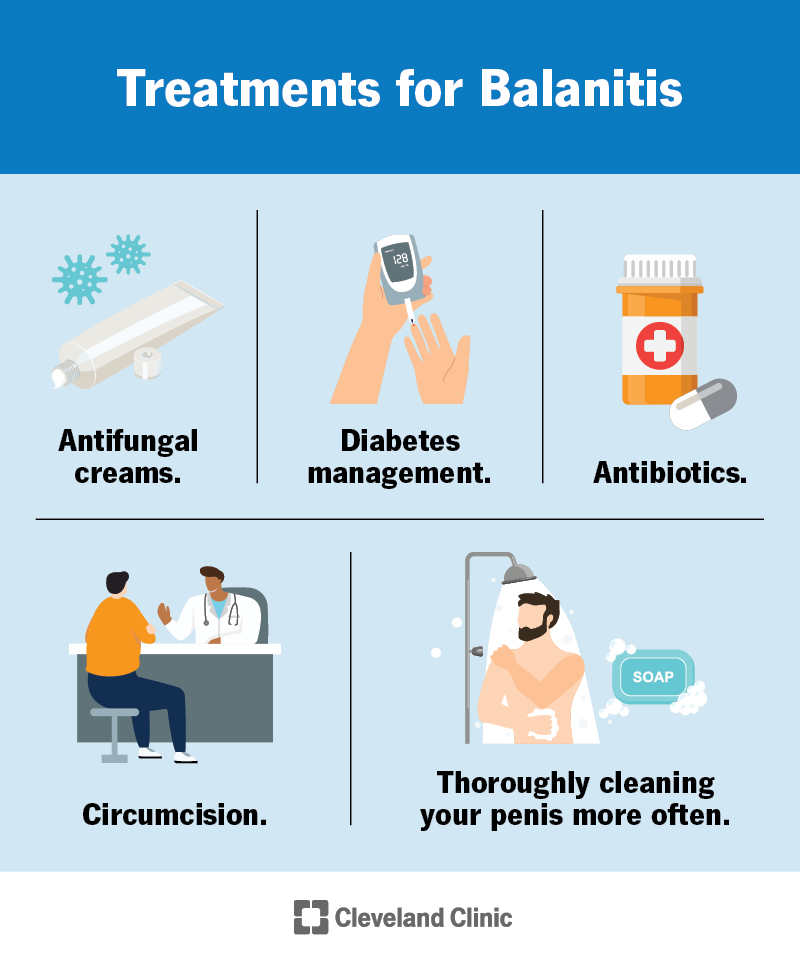
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21186-balanitis)
Balanitis is pain and inflammation (swelling and irritation) of the glans (head) of the penis that happens most often in uncircumcised males. Circumcision is a procedure that removes skin (the foreskin) from the head of the penis (glans). Yeast infections typically cause balanitis. However, bacterial infections, viral infections and some skin (dermatological) conditions can also cause balanitis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Balanoposthitis is inflammation of the foreskin and glans. This only occurs in uncircumcised males. Signs of balanoposthitis include itching, irritation and swollen foreskin and glans. Balanoposthitis occurs more often in people who have diabetes or a tight foreskin.
Balanitis looks like redness, discoloration (red, purple, gray or white) or discolored patches on the head of your penis. You may also have shiny, swollen areas of skin.
No, balanitis isn’t a sexually transmitted infection (STI), and it isn’t contagious. However, certain STIs may cause balanitis, and balanitis can look like an STI. Until you receive a balanitis diagnosis from a healthcare provider and they determine that its cause isn’t an STI, it’s a good idea to avoid having sex.
In most cases, balanitis isn’t serious. However, it’s important to see a healthcare provider to determine its cause and receive the proper treatment.
Most commonly, balanitis is due to an infection (fungal, bacterial, viral, parasitic). There are also some noninfectious types, which include:
Advertisement
There’s also a link to some types of balanitis and precancerous or cancerous conditions, including:
Healthcare providers estimate that up to 10% of males will have balanitis during their lifetime. Balanitis is more likely to occur in uncircumcised children under the age of 4. In adults, it’s more common if you have diabetes or if you have foreskin and don’t properly clean underneath it.
Symptoms of balanitis may appear suddenly or develop gradually. They can include:
If you have foreskin, the most common cause of balanitis is infrequently cleaning your penis and under your foreskin. Other causes include:
Balanitis primarily affects uncircumcised males because the moist, warm area under the foreskin is the ideal place for yeast and bacteria to grow. It can occur at any age and is more common in people who have tight foreskin that doesn’t easily move over the head of their penis (phimosis). Groups with a higher risk of balanitis include people who:
Untreated balanitis can cause chronic (long-term) inflammation. Lasting inflammation can lead to health issues, including:
Advertisement
Rarely, there’s a link between chronic inflammation and a higher risk of developing penile cancer.
Healthcare providers diagnose balanitis with a physical examination to determine if an infection is causing your symptoms. Your provider may swab your urethral opening (the hole at the tip of your penis) and send the sample to a lab for testing. Your provider may also order a urine test (urinalysis) or blood test to check for diabetes and other infections. Sometimes your provider may recommend a biopsy if they think you may have another condition that looks like balanitis.
If you have pain, irritation and discoloration on your penis, you may have balanitis. The risk increases if you have foreskin. See your provider for treatment and to determine what’s causing your symptoms. Other conditions (such as HIV, other sexually transmitted infections or a condition that’s likely to become cancer, called a premalignancy) can cause a rash and discoloration on the penis. It’s important to see your provider to get tested.
Advertisement
The treatment for balanitis depends on what’s causing the condition. Treatments can include:
Advertisement
Most cases of balanitis require some kind of treatment. If you don’t get treatment, your symptoms may get worse or you may develop more symptoms.
The fastest way to cure balanitis is to talk to a healthcare provider. They can make an official diagnosis, determine the cause and prescribe the best treatment.
To help quickly relieve swelling and pain, you can take over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen (Tylenol®). Not everyone can take these medications, so it’s a good idea to check with your healthcare provider. You can also apply ice or a cold compress wrapped in a light towel for up to 10 minutes several times a day to help reduce swelling.
In most cases of balanitis, you’ll start to feel better within a few days or a week after treatment.
With a proper diagnosis and treatment, you should make a full recovery.
Most people with balanitis recover with treatment. For people who have foreskin, it’s common for balanitis to return after treatment. The risk increases if you don’t clean under your foreskin regularly.
Preventing balanitis begins with practicing proper hygiene. To prevent balanitis, you should bathe often. Take the time to pull back your foreskin and clean the area underneath with warm water, and then dry it completely. Always use a condom when having sex to avoid contracting a sexually transmitted infection that can cause balanitis.
To ease the irritation and inflammation of balanitis, you should:
You should avoid having sex while you have balanitis, especially if you don’t know its cause. Sex can cause further irritation. If you have sex, wearing a condom may help protect your skin and reduce discomfort.
Even though balanitis isn’t an STI and your partner can’t catch it from you, it’s a good idea to be honest with them about it. If they have any questions, encourage them to talk to a healthcare provider.
If you have balanitis, masturbation can cause further irritation or discomfort. If you have pain, it’s a good idea to avoid masturbating until your penis has time to heal.
If you have symptoms of balanitis, you should visit your provider. Your provider will test you for infection and recommend good hygiene practices.
Herpes simplex 2 (HSV-2 or genital herpes) is an STI that causes painful sores on your genitals after you come in contact with the saliva (spit) or genitals of someone who has herpes. Genital herpes is a lifelong infection.
Balanitis isn’t an STI. It typically affects people who have foreskin, but it goes away with treatment. You can help prevent it from returning by regularly washing and drying the area or getting a circumcision.
Neosporin® (bacitracin, neomycin, polymyxin B) is a skincare ointment that helps prevent infections in minor scrapes or cuts on your skin. If a bacterial infection causes balanitis, Neosporin® may help kill the bacteria. However, in many cases, you may need an oral antibiotic.
Balanitis can affect up to 1 in 10 people who have a penis, and it’s more likely to occur if you have foreskin. It can be alarming, embarrassing and annoying, but it’s important to talk to a healthcare provider. They can help determine the cause and get you the proper treatment so it goes away. They can also help educate you on the best ways to prevent it from coming back.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When something’s wrong with your penis, you’ll want to get care right away. Cleveland Clinic’s experienced urology providers are here for you.
