Lissencephaly is a rare congenital condition that causes a developing brain to appear smooth instead of having normal bumps and folds. Lissencephaly is often caused by a genetic mutation, though non-genetic factors can also cause it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
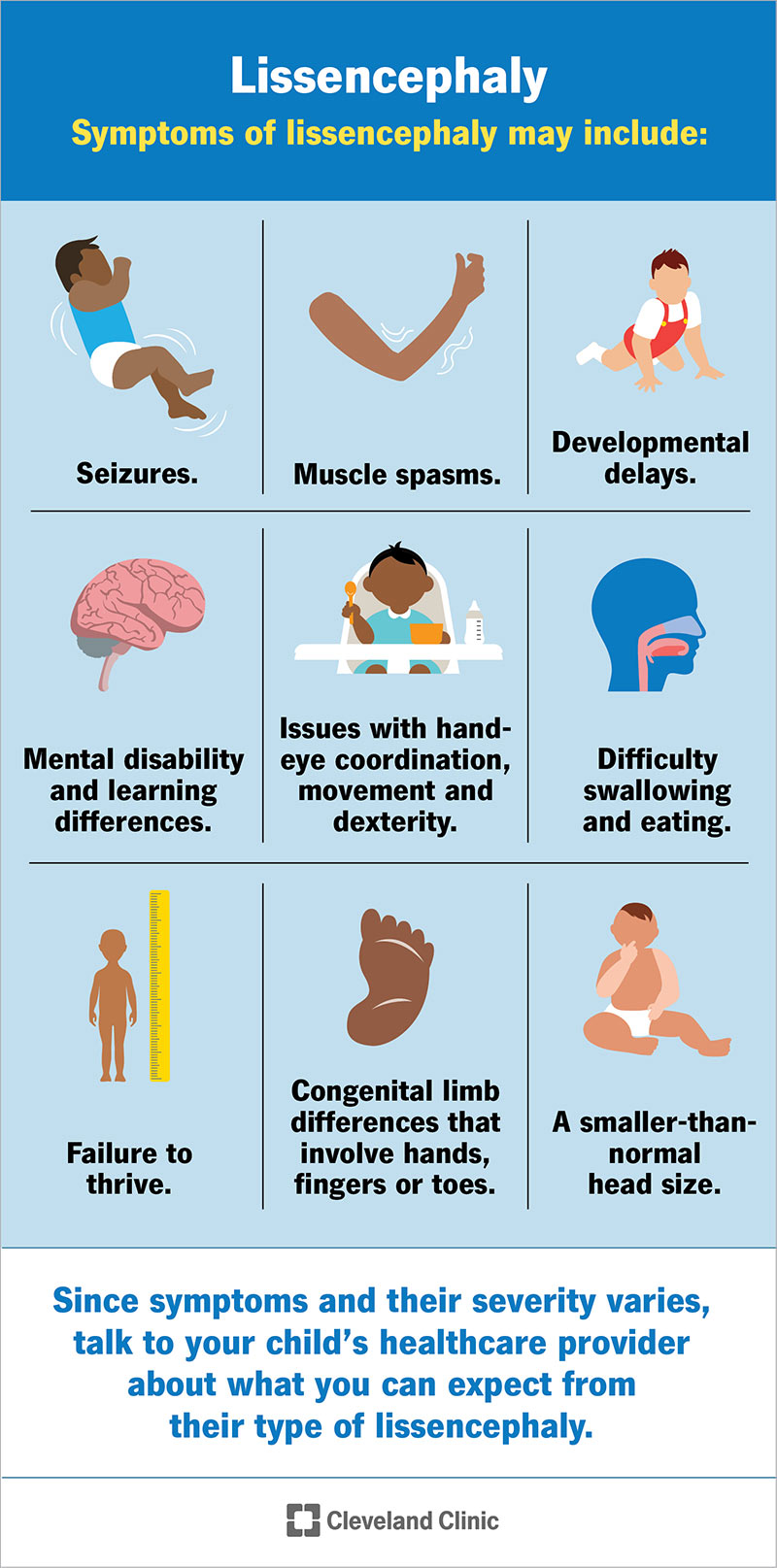
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/6033-lissencephaly)
Lissencephaly (pronounced li-suhn-SEH-fuh-lee), which means “smooth brain,” is a spectrum of severe and rare brain malformations (abnormally shaped) that affects developing fetuses. Gyri are the folds or bumps in your brain, and sulci are the indentations or grooves. In lissencephaly, the lack of normal development of brain gyri and sulci makes an affected baby’s brain appear smooth.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Gyri and sulci are important because they separate brain regions and increase your brain's surface area and cognitive ability.
There are more than 20 types of lissencephaly. Most of them are separated into two main categories: classic lissencephaly (Type 1) and cobblestone lissencephaly (Type 2). Each category shares similar symptoms but different genetic mutations.
Lissencephaly can occur on its own (isolated lissencephaly) or as part of certain syndromes, such as Miller-Dieker syndrome and Walker-Warburg syndrome.
Children with lissencephaly often have significant developmental delays and mental disability, but these vary from child to child depending on the severity of the condition.
Lissencephaly affects developing fetuses. It usually develops during the 12th and 24th weeks of fetal development during pregnancy and is often caused by genetic mutations (changes). In rare cases, it’s caused by non-genetic factors.
Lissencephaly is rare. Researchers estimate that lissencephaly affects about 1 out of every 100,000 babies.
Lissencephaly can cause a wide range of symptoms. It all depends on how severe the condition is and if it’s a part of a syndrome. Some children may develop as expected with a mild learning difference, while others may have many severe symptoms. The severity of symptoms can also vary widely.
Advertisement
Since symptoms and their severity can vary so much, it’s important to talk to your child’s healthcare provider about what you can expect from their type of lissencephaly.
Symptoms of lissencephaly may include:
Lissencephaly is caused by non-genetic and genetic factors and develops in fetuses between the 12th and 24th weeks of pregnancy.
These factors cause impaired neuronal migration of the outer region of the brain during fetal development. Your cerebral cortex, the part of your brain that’s responsible for conscious movement and thought, normally has several deep gyri and sulci (grooves and folds).
During fetal development, new cells that’ll later turn into specialized nerve cells normally migrate (travel) to the surface of the fetus's brain. This is called neuronal migration, and it results in the formation of several cell layers. These layers form gyri.
In cases of lissencephaly, the cells don’t migrate (travel) to where they’re supposed to, and the fetus doesn’t have enough layers of cells in their cerebral cortex. This causes a lack of or underdevelopment of gyri.
Non-genetic causes of lissencephaly include:
Genetic causes of lissencephaly are due to genetic mutations. A genetic mutation is a change in a sequence of your DNA. Your DNA sequence gives your cells the information they need to perform their functions. If part of your DNA sequence isn’t complete or is damaged, you might experience symptoms of a genetic condition.
A baby can inherit a genetic mutation from either or both of their biological parents, depending on how the mutation is passed down, but some mutations occur randomly with no previous history of the mutation in your family.
Scientists have discovered several gene mutations that can cause lissencephaly. Some of the affected genes include:
Advertisement
Healthcare providers can sometimes diagnose lissencephaly during pregnancy if they suspect the condition because of family history and/or prenatal ultrasound. They can diagnose lissencephaly through prenatal screenings, such as amniocentesis, and fetal magnetic resonance imaging (MRI).
Otherwise, providers typically diagnose lissencephaly at birth through physical evaluation and head imaging tests.
When diagnosing lissencephaly with imaging tests, providers look for a lack or reduction of the sulci and gyri (grooves and folds) on the surface of your baby’s brain and a thickened cerebral cortex.
If your healthcare provider suspects lissencephaly due to family history and/or the results of prenatal ultrasound, they may order specialized testing during pregnancy. These tests include:
Advertisement
Providers use the following imaging tests to help diagnose lissencephaly once your baby is born:
Your provider may also perform an electroencephalogram (EEG) on your baby. An EEG measures and records your child’s brain’s electrical signals. During an EEG, a technician places small metal disks (electrodes) on your child’s scalp. The electrodes attach to a machine that gives their provider information about your child’s brain’s activity.
To confirm the diagnosis, providers use DNA studies, such as chromosomal analysis and specific gene mutational analysis, to find the mutation responsible for lissencephaly.
Advertisement
There’s no cure or main treatment for lissencephaly. Instead, healthcare providers target treatment toward the specific symptoms that each child with lissencephaly has.
Treatment may require the coordinated efforts of a team of specialists, including:
Your provider will likely recommend genetic counseling if your child has lissencephaly.
The prognosis (outlook) for lissencephaly varies depending on the severity of the condition and if it’s part of a syndrome. Many children with lissencephaly remain at an early developmental level. But others develop normally with only mild learning differences.
Early and consistent therapy can be very helpful for some children. Therapies may include:
Most children with lissencephaly need daily medications to prevent seizures and treat other complications.
The life expectancy of lissencephaly is generally short. Many children with the condition die before they reach 10 years of age. The most common cause of death among people with lissencephaly is aspiration (breathing in a foreign object, such as sucking food into your airway) and respiratory disease.
It’s important to remember that no two children with lissencephaly are affected in the same way. It’s impossible to predict with certainty how your child will be affected. The best way you can prepare for the future is to talk to healthcare providers who specialize in researching and treating lissencephaly.
Unfortunately, most cases of lissencephaly can’t be prevented. If you plan on having a biological child, talk with your healthcare provider about genetic testing to understand your risk of having a child with a genetic condition or a condition that can be caused by an inherited genetic mutation, such as lissencephaly.
To help take care of your child with lissencephaly, follow their healthcare provider’s instructions for:
Lissencephaly can cause cognitive (intellectual), neurologic and/or psychomotor issues. Most children with lissencephaly will have problems with their development and may need help with daily tasks throughout their lives.
Your child’s healthcare team can answer questions and offer support. They also might be able to recommend a local or online support group.
If your child has been diagnosed with lissencephaly, they’ll need to see their healthcare team regularly to make sure their treatment is working and to assess their developmental progress.
Understanding your child’s lissencephaly diagnosis can be overwhelming. Your healthcare team will offer a robust treatment plan that’s unique to your child’s symptoms. It’s important to make sure your child is getting the love and support they need throughout their life and to stay attentive to their health to address any new symptoms that arise.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic Children’s offers compassionate, expert neonatal care and surgery for preemies and newborns with complex medical conditions.
