Papilledema is the medical term for swelling of the optic disc. It’s almost always bilateral (in both eyes). Papilledema can be very serious and must be treated.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
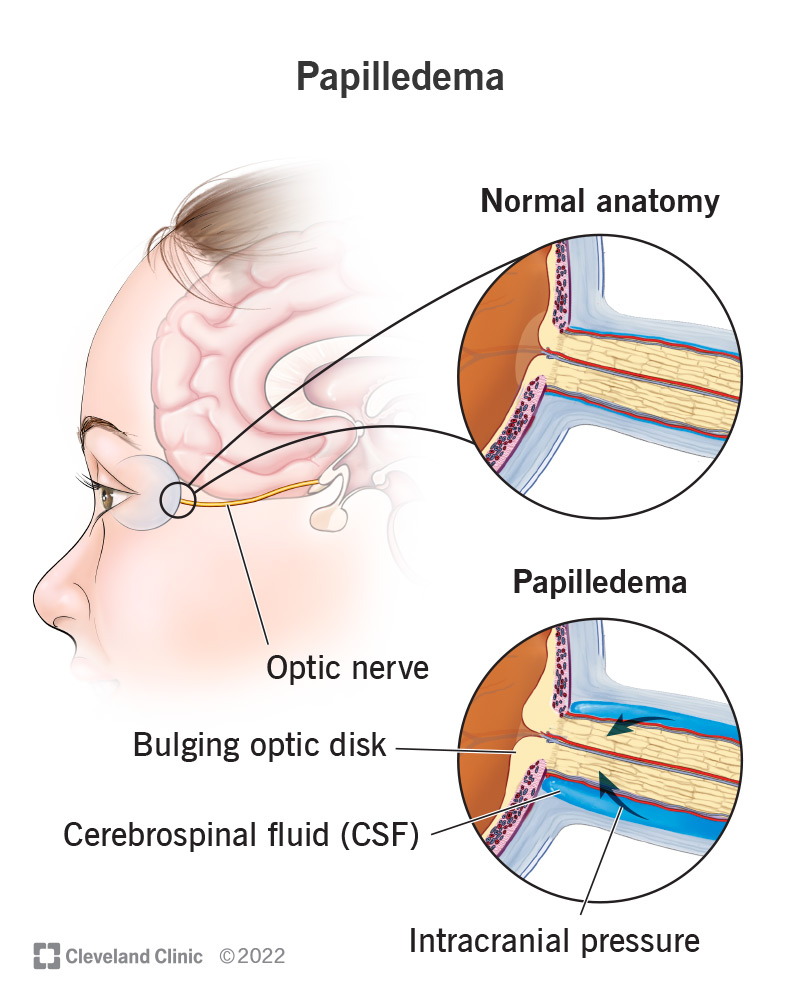
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24445-papilledema.jpg)
Papilledema refers to the swelling of both optic discs in your eyes due to increased intracranial pressure (intracranial hypertension). Cerebrospinal fluid (CSF) is constantly being released and then reabsorbed and normal levels help protect the brain from trauma.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The optic disc, or nerve head, is located where the optic nerve enters the back of the eye. The optic nerve is a pathway that connects the eye to the brain.
Intracranial hypertension usually results in bilateral papilledema (disc swelling of both optic discs). Swelling of the optic disc in only one eye (unilateral) is usually not the result of intracranial hypertension. Because of this, its name is optic disc edema.
Papilledema can be considered a medical emergency because intracranial hypertension can be serious, even potentially life-threatening.
Papilledema is more common in women. They’re usually 20 to 44 years old and are likely to have overweight (a BMI greater than 25) or obesity (a BMI greater than 30). The incidence of papilledema in this group is 13 per 100,000.
The incidence is much lower among other groups in the U.S. The incidence of papilledema among the U.S. population as a whole is 0.9 per 100,000 people.
You may have no symptoms (be asymptomatic), though you may have:
Advertisement
The vision loss worsens as the condition progresses.
High intracranial pressure causes papilledema. Related issues may include:
Papilledema isn’t hereditary.
Migraines don’t cause papilledema.
You may find out you have papilledema while your provider is evaluating you for other conditions, like illnesses that cause headaches and vision problems.
Your eye doctor will perform an eye exam with additional tests that may include visual field testing. They’ll be able to see if your optic disc looks swollen.
If your optic disc seems to be swollen, your provider will send you for an imaging examination, most likely a magnetic resonance imaging (MRI) scan.
Your provider may order a lumbar puncture (spinal tap).
Other tests may include blood tests to determine levels of iron and other substances in your blood.
Providers might use a version of the Frisén scale to grade or stage papilledema (that rates severity). The stages run from Grade 0 where the disc is normal but the edges may be blurred to Grade V where the whole disc is elevated, and you can’t see the blood vessels in the disc or those leaving the disc.
For papilledema due to idiopathic intracranial hypertension, your provider may prescribe a carbonic anhydrase inhibitor such as acetazolamide. They may also work with you to achieve and maintain a healthy weight as a long-term strategy.
If these methods don’t work, your provider may suggest surgical procedures to relieve and decrease intracranial hypertension.
For papilledema due to other causes, your provider will treat the underlying cause.
It’s important to treat papilledema because untreated papilledema can lead to partial or complete blindness in one or both eyes.
If you and your provider catch papilledema early, the outlook is good. Your provider will treat the condition primarily by addressing the issue that caused it.
It’s important to treat papilledema because of the potential for blindness and other neurologic effects.
Advertisement
You can reduce your risk of developing papilledema by:
Regular eye exams are important. As with most medical conditions, early diagnosis leads to better outcomes.
If you have new or worsening headaches, along with nausea and vomiting, you should seek immediate medical care. You should have any change in your vision assessed by a healthcare provider.
Pseudopapilledema means false papilledema. In pseudopapilledema, the optic disc looks elevated, but it’s not because of optic nerve swelling.
The causes of papilledema can be dangerous. It’s important to seek medical care if you experience any changes in vision, particularly if they occur in association with headaches, nausea and vomiting. Your provider will diagnose the cause and help you find the right treatment.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s ophthalmologists and optometrists have the highest training available. We provide exams, vision correction and care for many eye conditions.
