Thrombophlebitis is vein inflammation that happens in connection with one or more blood clots. This usually happens in your legs but can affect any vein in your body. While it isn't usually dangerous on its own, it's an important indicator of clotting problems that can lead to life-threatening conditions like pulmonary embolism.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
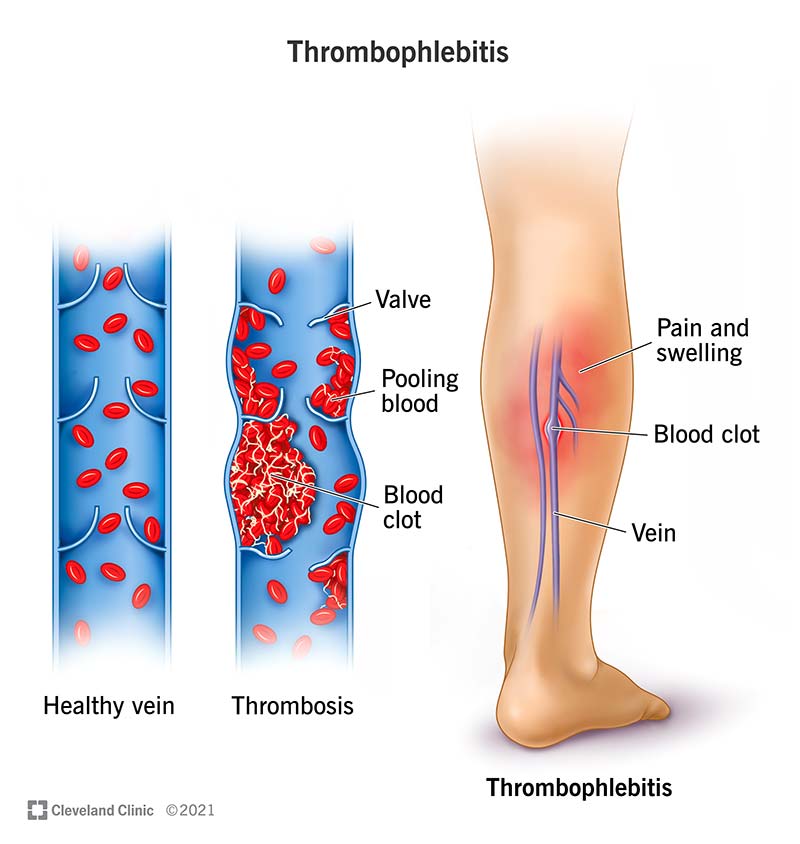
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/23311-thrombophlebitis)
Thrombophlebitis is a condition where you have pain and swelling that happen in relation to a blood clot in one of your veins. It most often happens in veins in your legs but can happen in any vein in your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Depending on why it occurs, how severe it is and where it happens, this condition can sometimes indicate a serious medical problem. Minor cases are typically treatable and not dangerous, but early detection and quick treatment are critical to avoid serious complications in more severe cases.
The name thrombophlebitis, pronounced “thromb-oh-fleb-eye-tiss,” breaks down into the following component terms:
Instead of being a one-way process, thrombophlebitis is more like the chicken and the egg question. It can happen in either of the following ways:
Thrombophlebitis is often a localized problem, meaning it commonly affects just one specific place in your body. However, the condition becomes much more serious if it spreads. Depending on where the initial clot forms, it can sometimes progress into dangerous and complicated conditions like deep vein thrombosis (DVT) or pulmonary embolism.
Advertisement
There’s a relationship between thrombophlebitis and thrombosis, but they aren’t the same thing. Thrombosis is when a blood clot forms inside one of your blood vessels. That means thrombophlebitis is a related process that sometimes — but not always — happens with thrombosis.
Thrombophlebitis can happen in any vein in your body. However, several named conditions involve thrombophlebitis that happens for a specific reason or in a certain place. Some of those named conditions include those listed below.
DVT is when a blood clot happens in a major vein, usually one in your legs. DVT is a serious condition that needs immediate treatment because it can lead to pulmonary embolism, a life-threatening medical emergency.
Superficial thrombophlebitis happens in smaller veins (or branches of the main veins) in your arms or legs. These are rarely as severe as DVT, but it can be a sign that there’s potential for DVT to happen. Superficial thrombophlebitis can also lead to other serious conditions.
As the name suggests, migratory thrombophlebitis is a condition that happens when a blood clot and related inflammation affect one vein (or a group of veins) and then migrate (move) onto any other vein(s). In some cases, this can involve multiple clots and may happen in multiple veins in your body at the same time. With this, a blood clot can move from a small vein into a larger one and put you at risk for more serious complications like pulmonary embolism.
This is when thrombophlebitis causes or happens because of an infection. When this kind of infection happens, it can lead to serious conditions, some of which include:
Septic thrombophlebitis is also especially dangerous because it may mean an infection is spreading throughout your body. That can cause sepsis, which is when your immune system dangerously overreacts to an infection spreading through your body. Sepsis is an extremely deadly medical emergency that needs quick diagnosis and rapid treatment.
Thrombosis is possible at any age, especially in people with certain health conditions or life circumstances. However, your risk for developing this condition starts to increase at age 45 and will continue to increase as you get older.
Advertisement
Depending on the specific type of thrombophlebitis, this condition ranges from rare to relatively common. Perhaps the most common and well-known example of a related condition is deep vein thrombosis. Each year in the United States, there are an estimated 900,000 cases of DVT, resulting in about 60,000-100,000 deaths per year.
Thrombophlebitis almost always involves the following symptoms:
Advertisement
Other symptoms that can — but don’t always — happen include:
Thrombophlebitis can happen for several different reasons. The following may cause blood clots to form or may merely make them more likely.
Advertisement
While it sometimes happens because of an infection, thrombophlebitis is not a contagious condition on its own. This also applies to genetic conditions, which pass in DNA from parent to child. These conditions don’t cause thrombophlebitis directly, but they can cause clotting problems that can lead to this condition.
Healthcare providers usually diagnose thrombophlebitis in a hospital setting, especially in an emergency room. That's because thrombophlebitis has close connections to severe, potentially life-threatening conditions like DVT.
Your provider will diagnose thrombophlebitis based on a combination of a physical exam, imaging tests and lab tests. Combining these various methods is important because a physical examination alone is usually not enough to diagnose thrombophlebitis. Several conditions have similar symptoms, some of which are especially dangerous, which makes imaging and lab tests even more useful — if not critical — in preventing serious complications.
A variety of tests are possible when healthcare professionals investigate the possibility of thrombophlebitis or any related or similar conditions. These include:
In rare cases, migratory thrombophlebitis (mentioned above) can be a sign of certain types of cancers, especially cancers in your abdomen. That may lead healthcare providers to run tests that look for those kinds of cancers.
In cases where thrombophlebitis happens because of IV or catheter lines, removing that line is usually the first step. Other treatments usually involve the following.
Several different types of medications can help with the symptoms of thrombophlebitis and resolve the involved clot. These include:
In rarer cases, surgery is the best option to help treat severe thrombophlebitis (especially in your legs). Surgery can involve one or more of the following procedures:
Your healthcare provider may instruct you to wear compression items or clothing. These items, such as socks, stockings or wrappings/bandages, put consistent (but light) pressure on certain parts of your body. That pressure can help prevent new clots from forming and ease the pain and swelling from any previous clot(s).
The complications and side effects that are possible with thrombophlebitis treatments can take many forms. Your healthcare provider is the best person to tell you what risks are most likely with your particular case and what you can do to minimize the risks.
In many cases, the treatments mentioned before aren’t necessary. In those cases, your healthcare provider will likely recommend supportive treatments. These include:
The severity of your case and the treatments you receive determine when you feel better and how long it takes you to recover. In general, you should start to feel better while your symptoms are being treated, especially with medications that treat pain. Most people recover from thrombophlebitis within days, but some may need a little longer (especially if they had complications, the clot was in a critical location or they needed surgery).
Thrombophlebitis is a serious condition, but it doesn't usually cause problems on its own. It's usually an indicator of clotting problems that can cause more serious conditions, some of which are deadly. If caught early, thrombophlebitis is very treatable, and complications are rare. However, waiting to get this condition diagnosed and treated increases the risk of developing more serious problems.
Thrombophlebitis tends to be a short-lived condition, especially with quick diagnosis and treatment. It’s rare for it to last more than a few hours because the longer you have it, the greater the risk of it becoming a more dangerous problem.
On its own, thrombophlebitis is usually not dangerous. However, having it does mean you have a much higher risk of developing other conditions like DVT or pulmonary embolism, both of which are medical emergencies. The longer you wait to get treatment, the more dangerous this condition becomes. Waiting also increases the risk of developing long-term problems like chronic pain or scarring in the affected veins (which can limit blood flow).
The key to preventing thrombophlebitis is knowing you’re at risk for a clot to happen. If you know this, your healthcare provider can prescribe medications like blood thinners, which can stop a clot from forming in the first place.
Unfortunately, many potential factors can make prevention difficult or even impossible. One reason is not knowing you have a health condition (genetic or otherwise) that causes blood clots. Another example is when the clot is a rare complication of a common life circumstance, such as pregnancy.
There are several things you can do to reduce your risk of developing a clot and thrombophlebitis. The most important thing is to minimize or eliminate any risk factors that you can. The ones you can impact the most tend to include:
If you have conditions that increase your risk for blood clots and thrombophlebitis, the best thing you can do is manage those conditions. That includes:
You should always call your healthcare provider if you have any symptoms of thrombophlebitis. You should also call them if you have a history of thrombophlebitis (or other clotting problems like DVT) and any of your symptoms return or suddenly worsen.
You should go to the hospital immediately if you have any symptoms of blood flow blockage. If the blockage affects one of your limbs, these symptoms usually include:
Thrombophlebitis can be an important warning sign of much more serious conditions. While it isn't usually dangerous on its own, you need to see a medical professional to determine if you have a problem. You might also need to seek emergency care immediately with certain symptoms. With quick diagnosis and treatment, thrombophlebitis is less likely to cause major problems or disrupt your life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Vascular disease may affect your life in big and small ways. Cleveland Clinic’s specialists treat the many types of vascular disease so you can focus on living.
