Heel fad pad syndrome is the thinning of the fat pad that supports and cushions your heel. It’s a painful condition. Causes include high-impact activities, prolonged standing and walking, improper footwear or no footwear. Treatments include simple methods such as rest, ice and proper footwear to more advanced options such as fillers and fat grafting.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
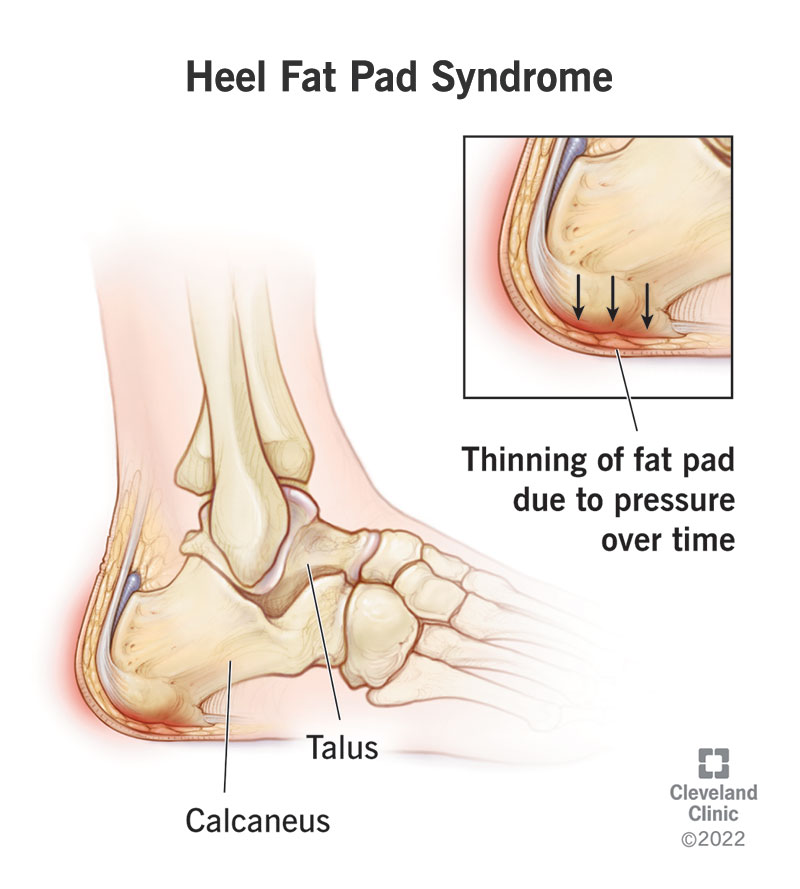
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23275-heel-fat-pad-syndrome.jpg)
Heel fat pad syndrome is the thinning of the fat pad on your heel.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your heel pad is made up of fatty tissue and thick elastic muscle fibers. Your fat pad acts as a shock absorber or cushion and a protector of your heel as you walk, run and jump. Over time, too much wear and tear on your heel pad and other factors cause the fatty tissue to shrink or cause the heel pad tissue to lose its elasticity. The result is heel pain that can interfere with your daily routine and activities.
Heel fat pad syndrome is also known as fat pad atrophy, fat pad syndrome and heel fat pad atrophy.
Heel fat pad atrophy is considered the second leading cause of plantar heel pain after plantar fasciitis. Heel fat pad syndrome is often misdiagnosed as plantar fasciitis.
Symptoms of heel pad syndrome include:
Mild cases may not have symptoms or you may only notice occasional pain when walking barefoot or on a hard surface, running or when pressing your fingers into the middle of your heel.
Advertisement
Heel fat pad syndrome is a wear and tear condition. Many factors contribute to it, including:
Medical conditions that contribute to the development of heel fat pad syndrome include:
Your healthcare provider will ask about your medical history and your current symptoms.
Your provider will ask you detailed questions about your heel pain including:
Your provider will perform a physical exam of your foot, looking for structural problems and will attempt to reproduce your pain by pressing on the center of your heel. Your provider will also compare the thickness of your heel pad when you’re standing on your foot compared with when you’re not. Normal heel pad thickness is 1 to 2 centimeters (0.4 to 0.8 inches). A stiff, hard heel pad may mean your heel doesn’t have a lot of elasticity, which is a sign of heel fat pad syndrome.
Advertisement
Your provider may also order an X-ray, ultrasound or sometimes magnetic resonance imaging (MRI) to help make the diagnosis of heel fat pad syndrome or to rule out other causes of your heel pain.
Treatments include conservative approaches and more advanced techniques. The goal of conservative treatment is to reduce pain and inflammation, preserve and protect the fatty tissue that’s present and prevent further damage. Advanced treatment methods add materials to your heel to increase the thickness of your heel pad.
Conservative treatment methods include:
Advertisement
Advanced treatment methods include:
Surgery may be considered to correct physical deformities in your toes, foot, ankle, leg, knee or hip that change your alignment and weight distribution and affect the quality of your life or limit your abilities.
Advertisement
If you leave heel fat pad syndrome untreated, you’ll:
There’s no absolute long-term cure for heel fat pad syndrome. There’s some degree of shrinkage of your heel fat pad that occurs with ordinary aging and natural wear and tear. However, by taking steps to reduce heel pain and inflammation and prevent further damage you can improve the quality of your life and continue to engage in activities that bring you joy.
Although wear and tear from increasing age or a family history of this condition can’t be prevented, you can focus on certain lifestyle habits to lower your chance of developing heel fat pad syndrome. These include:
Inspect all your shoes. Change your shoes if you see uneven wear on the soles or inside cushioning that’s no longer supportive.
Plantar fasciitis is a weakening of the connective tissue (the fascia) that supports the arch of your foot. Your plantar fascia stretches from your heel to your toes. The main symptom of plantar fasciitis is a throbbing pain in your heel. The pain is usually closer to your instep or inner part of your heel and may extend to your foot’s arch. You feel a tightness in the bottom of your foot when stretching. Also, the pain is worse in the morning with first steps after rest, improves after use but then worsens with continued weight-bearing on your foot. The pain is described as sharp and stabbing if the plantar fascia is pressed on during examination.
The pain of heel fat pad syndrome is closer to the center of your heel. Pain happens when walking or standing for long periods, when participating in high-impact activities and is aggravated with walking barefoot on hard surfaces. The pain in your heel may happen more often at night and at rest and is more likely to happen in both feet compared with plantar fasciitis.
You can have both conditions at the same time. Also, having plantar fasciitis can lead to heel fat pad syndrome. This happens because when the plantar fascia is injured, it reduces the ability to properly distribute weight on your foot when walking or running. This leads to extra pressure on your heel fat pad and quicker wearing.
Your heel bone is called the calcaneus. Repetitive movements that overload weight on your heel, such as running, can cause your calcaneus to crack. This crack or break is called a stress fracture. If you have a calcaneal stress fracture, you’ll feel pain in your heel as well as at the back of your heel. The heel pain worsens over time, first starting only when engaged in activities and then later even when you are resting your foot. A bone scan, computed tomography (CT) scan or magnetic resonance imaging (MRI) scan may be needed to determine if your heel pain is due to a stress fracture.
Heel fat pad syndrome is the loss of the thickened, cushioning pad on the heel area of the sole of your feet. This heel pad loses its density and elasticity due to wear and tear, repetitive activities that apply a lot of stress to your heel pad, heavier body weight, unequal distribution of your weight when you walk and other factors. The main symptom is deep pain in the center of your heel. Simple treatments, including rest, anti-inflammatory medication, ice and proper footwear can usually manage heel fat pad syndrome. Other advanced treatments are available and may be an option. Always see your healthcare provider if you experience heel pain. The earlier the problem can be diagnosed, the early treatment can begin, which leads to less damage and a better outcome.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
An aching foot or heel can bring your favorite activities to a halt. Cleveland Clinic’s foot pain experts are here to help you heal and get back on your feet.
