Tinea capitis, or scalp ringworm, is a fungal infection that affects your child’s scalp and hair. Symptoms of tinea capitis include swollen red patches, dry scaly rashes, itchiness and hair loss. Mold-like fungi called dermatophytes cause tinea capitis. Treatment for a tinea capitis infection involves the use of an oral antifungal medication.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
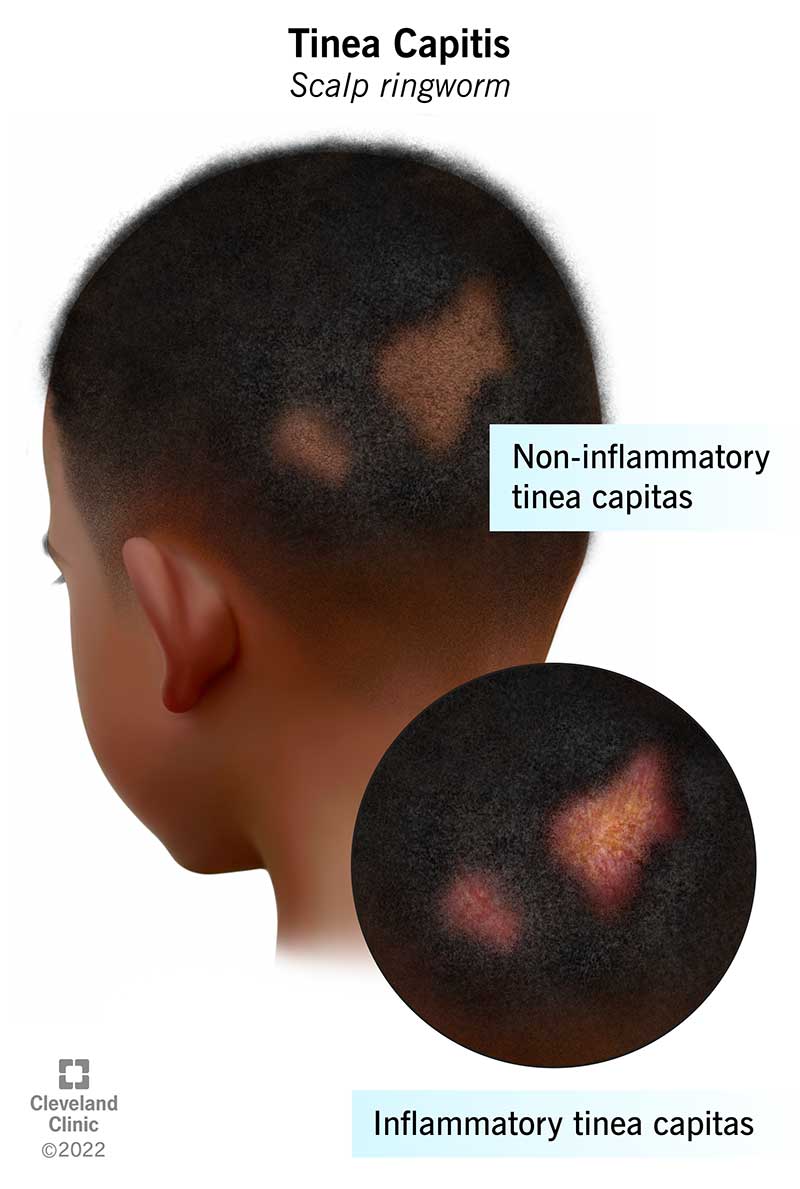
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22449-tinea-capitis)
Tinea capitis is a fungal infection that affects your child’s scalp and hair. Another name for tinea capitis is scalp ringworm. Tinea capitis occurs when fungi enter your child’s hair follicles and often hair shafts. Tinea capitis may also affect your child’s eyelashes and eyebrows.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Tinea capitis can be inflammatory or non-inflammatory. The inflammatory type can cause kerion. Tinea capitis kerion are painful, pus-filled patches that sometimes ooze. A reaction to the fungus in your child’s immune system causes kerion. It may cause scarring and permanent hair loss.
The non-inflammatory type of tinea capitis doesn’t usually cause permanent hair loss. It can cause black dot tinea capitis, which means your child’s hair shafts break at their scalp surface. Gray patch tinea capitis is another type of non-inflammatory ringworm. It means your child’s hair shafts break above the surface, leaving short stubs.
Tinea capitis most commonly affects children between the ages of 3 and 14. But tinea capitis occurs in adults as well. It's especially common in people with weakened immune systems.
Tinea capitis is a common condition primary care providers and dermatologists see. Diagnosis of the infection happens all over the world. It’s most common in hot, humid areas such as Central America, Southeast Asia and Africa.
Tinea capitis may affect all or part of your child’s scalp. Symptoms may include:
Advertisement
Inflammatory tinea capitis can cause painful swollen patches on your child’s scalp. These patches are called kerion. The kerion may have crusty blisters and ooze pus. Inflammatory tinea capitis may cause scarring and your child’s hair may not grow back.
Black dot tinea capitis causes hair shafts to break at the surface, which look like black dots. Gray patch tinea capitis leaves short hair stubs.
Mold-like fungi called dermatophytes cause tinea capitis. In the United States, dermatophytes called Microsporum and Trichophyton are the most common causes of the infection. Fungi thrive in warm, moist environments. It commonly grows in tropical places.
Tinea capitis also spreads very easily. Your child can get tinea capitis from contact with infected people, animals and soil. They can also get it by using objects and touching surfaces that harbor the fungus. Tinea capitis can live for a long time on infected objects and surfaces.
Tinea capitis grow and thrive in moist, warm environments. The most common risk factors include:
Tinea capitis is very contagious. It can spread quickly among children. Tinea capitis spreads mainly through one of three ways.
Your child can get tinea capitis after direct contact with someone who has the infection. The person may or may not have symptoms. But if they’re a carrier of the infection, they can spread it.
Your child can get tinea capitis after touching an animal that has the infection. Many different animals can spread tinea capitis. This includes pets such as dogs and cats.
Fomites are objects or materials that are likely to carry an infection. Your child can get tinea capitis by sharing clothes, hats, combs, hairbrushes and helmets.
Your child’s healthcare provider will ask about their symptoms. They’ll also perform a physical examination. They’ll look at your child’s hair, skin and scalp. They may be able to tell it’s ringworm just by looking at it.
Your child’s healthcare provider may want to collect a sample of the infected area. They’ll pluck some hairs and/or take a small scraping of your child’s scalp. They may want to order other tests to confirm a tinea capitis diagnosis.
To confirm a tinea capitis diagnosis, your child’s healthcare provider may order a test.
Advertisement
Your child’s healthcare provider will gently scrape some of the skin from the infected area of your child’s scalp. They may also pluck some hairs. In a lab, a technician will place the samples onto a microscope slide. The slide contains a drop of potassium hydroxide (KOH). They’ll look at the samples under a microscope. The KOH stain makes it easier for the technician to see if there’s a fungus present. The results are generally back within 24 hours.
If the KOH stain doesn’t provide accurate results, your child’s healthcare provider may order a culture. A culture is a substance that allows fungi to grow. The technician can then identify the fungus causing your child’s infection. A culture is more accurate and specific than a KOH stain, but it can take several weeks to get the results.
A Wood light is a special type of ultraviolet (UV) light. Your child’s healthcare provider will shine a Wood light onto your child’s scalp. They may be able to determine the type of fungus causing the ringworm. Sometimes ringworm glows under UV light when other rashes don’t. Depending on the dermatophyte present, the area on your child’s scalp may glow a yellow, green or blue color.
Your child’s healthcare provider may prescribe an antifungal medication to treat tinea capitis. Topical treatments usually don’t work, so they’ll prescribe a medication taken by mouth. Your child will have to take the medication for at least six weeks. Oral antifungal medications for children include griseofulvin and terbinafine.
Advertisement
Your child’s healthcare provider may prescribe a selenium sulfide shampoo. You’ll need to wash your child's hair with the shampoo at least twice a week. This shampoo may help prevent tinea capitis from spreading, but it won’t cure tinea capitis.
Your child’s healthcare provider may also recommend an antifungal cream. You'll apply the antifungal cream directly onto your child’s scalp. Antifungal creams can help prevent the infection from spreading. But they won’t cure tinea capitis.
If your child has kerion, their healthcare provider may prescribe a corticosteroid such as prednisone. Steroids may help reduce inflammation and lower the risk of scarring and permanent hair loss.
Treatment for tinea capitis in adults includes oral antifungal medication as well. You’ll need to take the medication for at least six weeks to make sure the infection clears completely. Oral antifungal medications for adults include terbinafine and itraconazole. Your healthcare provider may also recommend selenium sulfide shampoo, antifungal creams and steroids.
If you or your child have tinea capitis, you should check everyone else in your household for the infection. You may want to treat them even if they don’t have symptoms. If not, everyone could continue to pass the infection back and forth among each other. Children can use antifungal creams or shampoos twice a week for at least six weeks.
Advertisement
In addition, you should wash pillows, bedding and towels thoroughly. You should clean, disinfect and/or replace any shared combs, brushes and other hair equipment.
Non-inflammatory tinea capitis has a good prognosis with early and persistent treatment. But tinea capitis can be hard to cure. It’s important your child completes their antifungal medication treatment. Severe inflammatory tinea capitis can cause areas of scarring and permanent hair loss.
Fungal infections can be difficult to cure. It’s important your child uses their antifungal medication as directed. They may need to use an antifungal medication consistently for at least six weeks. Your child’s infection may look like it’s going away or even gone, but it will come back if the infection isn’t treated completely. Often, tinea capitis gets better on its own after puberty.
There are many steps you can take to prevent tinea capitis. These steps include:
Seborrheic dermatitis is a common skin condition that occurs more often in older children. Unlike tinea capitis, it doesn’t cause hair loss. In some cases of tinea capitis, the lesions look like those seen in seborrheic dermatitis. But in seborrheic dermatitis, the hairs aren’t broken. You may be able to treat seborrheic dermatitis with over-the-counter treatments. But tinea capitis generally requires a prescription medication.
Tinea barbae is a fungal infection like tinea capitis, but it affects the beard and mustache areas of your face. It’s less common than tinea capitis and generally only affects adult males. Tinea barbae most commonly affects farmers. The infection spreads through direct contact with an infected animal. It very rarely spreads from person to person.
Tinea capitis infections can be itchy and uncomfortable for your child. With early and persistent treatment, you should be able to help clear up your child’s infection. But it can take some time. It’s important to follow your child’s healthcare provider’s instructions. Your child needs to complete the treatment. It can take at least six weeks for a fungal infection to clear. If the infection isn’t going away, reach back out to your child’s healthcare provider. They’re there to help you and your child.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
As your child grows, you need healthcare providers by your side to guide you through each step. Cleveland Clinic Children’s is there with care you can trust.
