Vulvar varicosities are swollen veins on your vulva that usually show up when you’re pregnant. You can have them without having any symptoms. Or you may notice signs that they’re there, like pain or a feeling of fullness in your vulva. They usually go away once your baby is born. In the meantime, you can manage symptoms at home.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
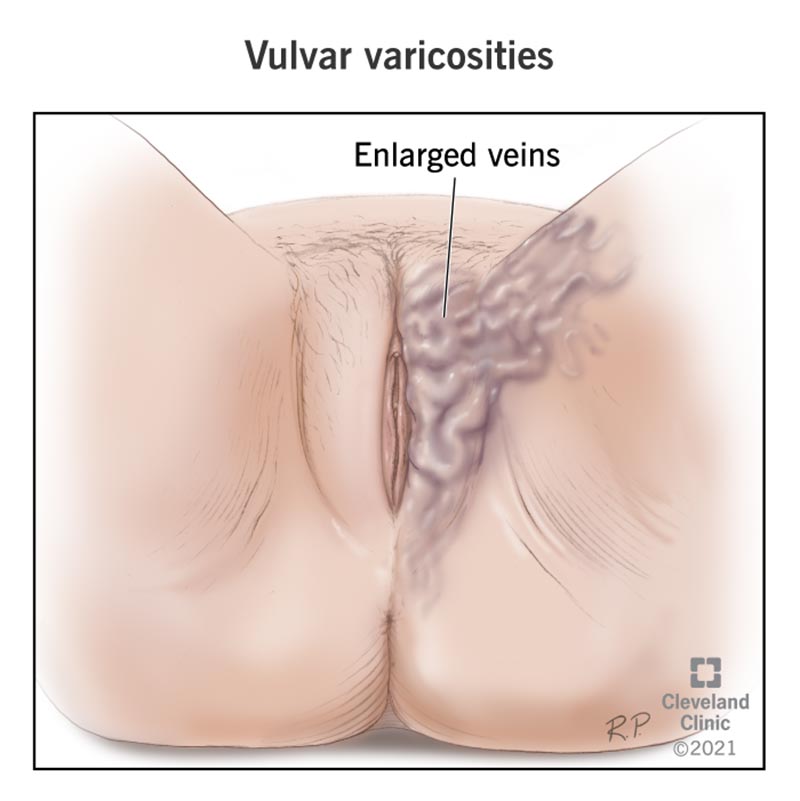
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22127-vulvar-varicosities)
Vulvar varicosities are varicose veins that appear on your vulva (external female genitals). They usually show up during pregnancy, when your blood volume increases significantly to support a growing fetus. These changes in blood flow during pregnancy can cause the veins in your genital region to become swollen.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Vulvar varicosities typically appear in the third or fourth month of pregnancy. Vulvar varicosities can be uncomfortable, but they shouldn’t affect your labor or delivery. They usually go away without treatment about six weeks after your baby is born.
It's rare to get vulvar varicosities when you're not pregnant. This is more likely if you have varicose veins in other places on your body (like your pelvic or groin area).
About 4% of people with vulvas have vulvar varicosities. That number goes up to 20% for pregnant women. It’s rare to have a severe case of vulvar varicosities, even during pregnancy.
You may not notice any symptoms with vulvar varicosities. Or you may notice that your vulva feels swollen and uncomfortable. Some other symptoms are:
Vulva varicosities can appear alone or along with varicose veins in your legs, calves or upper thighs.
You may notice bluish or purplish veins that pop out beneath your skin. Other than bulging veins, your veins may also appear twisted, swollen or bunched into a cluster.
Possibly. Skin irritation and itchiness can be a symptom of vulvar varicosities.
Advertisement
Yes, they can. Rarely, the veins can burst (or rupture) during a vaginal delivery. The bleeding is usually mild, and your provider can control it without it causing problems.
Not all of them hurt, but some do. Vulvar varicosities don’t feel the same way for every person. Your veins may feel mildly uncomfortable, or the pain may be severe. Whether your veins feel painful or not, it’s a good idea to let your provider know about them.
Vulvar varicosities appear when the veins in your vulva struggle to circulate blood. These veins move blood from your lower body and your pelvis up — against gravity — to your heart. When they’re able to keep the blood flow steady, you likely won’t even notice these veins doing this important work. When there’s more blood to move than these veins can handle, the blood starts to pool (or collect) and swell in your veins.
Your body goes through changes during pregnancy that increase your chances of getting vulvar varicosities, like:
Experts know less about what causes vulvar varicosities in people who aren’t pregnant. It’s likely that your genetics influence how well your veins manage blood flow.
Being pregnant is the biggest risk factor for vulvar varicosities. The increase in blood flow, hormones and the heaviness of your uterus make you more prone to them. Other things that increase your risk are:
There aren’t any life-threatening or long-term complications of vulvar varicosities. Potential complications are:
Advertisement
Your healthcare provider will do a physical exam to see if you have vulvar varicosities. As part of the exam, your provider may take a closer look at your vulva while you’re lying down and while you’re standing. Viewing your vulva from both these angles can help your provider compare how your veins look without pressure (lying down) and with pressure (standing up).
Your provider may order an imaging procedure to check the size of your veins and to track how well your blood circulates through your veins. Imaging can also let your provider know if your varicose veins are only in your vulva or if you have varicose veins in other parts of your pelvis, too. Your provider can use this information to recommend treatment.
If you’re pregnant, vulvar varicosities will likely go away after your baby’s born, so your best treatment approach may be managing symptoms. If you still have them a few months after you give birth, your provider will recommend treatment.
If you’re not pregnant, your provider can work with you to determine what’s likely causing your swollen veins. The treatments they suggest will depend on what’s causing the swelling and whether other veins in your pelvis and legs are also affected.
Advertisement
Potential treatments for vulvar varicosities are:
Your provider can help you weigh the potential benefits associated with these procedures against more conservative treatments, like managing symptoms.
Vulvar varicosities usually go away six weeks after you’ve had your baby. In the meantime, keep the following in mind as you manage your symptoms:
Don’t:
Do:
Advertisement
There are support garments exclusively for people with vulvar varicosities, similar to compression socks for your legs. They work by compressing your veins, which can help with swelling and discomfort.
Walking helps get the blood circulating throughout your body. Just take care not to overexert yourself. Too much activity can make your veins feel more painful.
If you’re pregnant, you can expect the veins in your vulva to go back to normal about six weeks after you deliver your baby. The symptoms can be frustrating, but vulvar varicosities don’t cause pregnancy complications. You should be able to deliver your baby vaginally, with no risks to your baby.
If you’re not pregnant, work with your provider to monitor your veins and discuss treatment options.
Try not to worry about vulvar varicosities. They often disappear entirely a few weeks after you deliver your baby. If you have severe symptoms or they don’t go away after delivery, your healthcare provider can recommend treatment. Always let your healthcare provider know about your symptoms so they can monitor you and watch for any complications.
You can’t prevent vulvar varicosities. But you can do things to improve your circulation overall so that blood flows better throughout your entire body:
Let your provider know about any issues you’re having with your circulation, including vulvar varicosities. Also, your provider can help you manage symptoms and offer treatment options.
Deep vein thrombosis (DVT) is a serious blood clot that’s rare among people with vulvar varicosities. Still, it’s a good idea to know what the symptoms are, just in case. See your provider right away if you notice that your veins have become:
It’s very rare to get vulvar varicosities when you’re not pregnant. But the changes that occur during your menstrual cycle may worsen your symptoms.
Noticing enlarged veins on your genitals can feel embarrassing. Feeling itchiness, fullness or pain in your vulva at the very moment that you’re noticing these veins may add insult to injury. Take comfort in knowing that the changes are likely short-term. Many at-home treatments may make it easier to manage your symptoms. And if they’re still around after your baby comes, your healthcare provider can recommend additional treatments that can bring you relief.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
From routine pelvic exams to high-risk pregnancies, Cleveland Clinic’s Ob/Gyns are here for you at any point in life.
