Ventricular arrhythmias are abnormal heart rhythms that make the lower chambers of your heart twitch instead of pump. This can limit or stop your heart from supplying blood to your body. While some of these arrhythmias are harmless and don’t cause symptoms, some can have serious — or even deadly — effects on your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
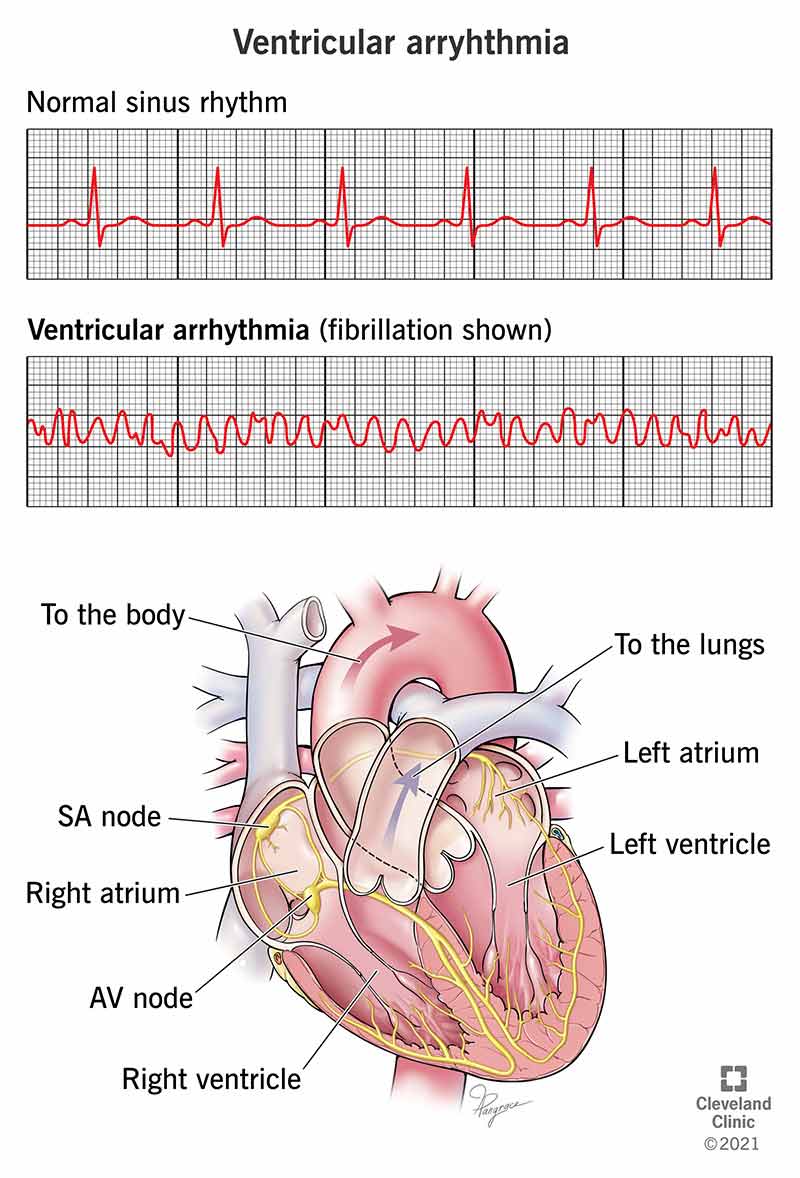
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21854-ventricular-arrhythmia-illustration)
A ventricular arrhythmia is an abnormal heart rhythm that affects just the lower chambers of your heart. Those lower chambers are what drive the heart’s ability to pump blood throughout the body. While some of them are harmless and don’t usually cause symptoms, some of these rhythm problems can have serious — or even deadly — effects on your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your heart is a pump that has four chambers. The upper chambers are the left atrium and right atrium (you can say “atria” to refer to both of them). The lower chambers are the left ventricle and right ventricle.
The right ventricle pumps blood out of your heart and into your lungs, which add oxygen and remove carbon dioxide before the blood reenters your heart. The left ventricle is the last chamber blood flows through before being pumped out to your entire body.
Because the ventricles are so key to the heart’s ability to pump blood, any disruption in their normal rhythm can have major consequences. These include:
Without CPR or the use of an automated external defibrillator, both of these conditions are deadly within minutes.
There are three main types of ventricular arrhythmias: Preventricular contractions, ventricular tachycardia and ventricular fibrillation.
Also known as PVCs, these feel like extra heartbeats and are usually harmless. A key exception is when you have a condition that has changed the shape of your heart or when PVCs happen frequently or for longer periods.
Advertisement
Ventricular tachycardia (VT) happens when the lower chambers of the heart beat unusually fast. This can happen because of a malfunction in the heart's electrical system. In some cases, VT can turn into ventricular fibrillation, which is a more dangerous condition.
The following features can distinguish different types of VT:
Under normal circumstances, the waves that show your heart activity are organized and follow a pattern called “sinus rhythm.” When your heart doesn’t follow that pattern, healthcare providers will look at the shape of the pattern for clues to help them figure out the problem.
Changes that clinicians look for include:
Ventricular fibrillation — often shortened to “v-fib” — happens when the lower chambers of the heart quiver or twitch rather than expand and contract. Because the ventricles don’t fully expand and contract, blood doesn’t get pumped through them. This causes your heart to stop, sending you into sudden cardiac arrest, and lack of blood flow to your brain causes you to pass out within seconds. If blood flow isn’t restarted within a few minutes, this condition is deadly.
The symptoms of ventricular arrhythmia depend on the type of arrhythmia. Some have no symptoms (especially non-sustained and benign arrhythmias).
Ventricular tachycardia usually has the following symptoms:
Ventricular fibrillation typically causes a person to collapse or pass out. Sometimes, there are no warning signs before this takes place. If symptoms happen, they tend to appear just minutes before a person passes out. Symptoms often include:
Advertisement
Ventricular tachycardia causes include:
Ventricular fibrillation causes include:
Ventricular arrhythmias are most common in people who have heart-related conditions and diseases. As a result, the likelihood of developing these arrhythmias naturally increases as you get older. In addition, diseases that change the heart's structure have a much higher risk of causing ventricular arrhythmias.
Ventricular arrhythmias happen to millions of people each year. Some of these happen to people of all ages and are harmless.
Sustained ventricular arrhythmias — which are more likely to be harmful — are very common. They’re most likely to happen in people with underlying heart problems. However, they can also happen in people with no symptoms or who have no idea they have a heart condition. An estimated 180,000 to 450,000 sudden cardiac deaths happen each year in the United States. Of those, a significant portion may occur because of sustained ventricular arrhythmias.
Advertisement
A healthcare provider will often begin diagnosing an arrhythmia based on your symptoms and by asking you questions. These help the provider build what's called a "patient history." Think of a history like a file a detective builds while solving a mystery. The more clues collected, the easier it is to crack the case.
Your primary care provider or a specialist will likely start with a physical exam. This includes listening to your heartbeat, measuring your blood pressure and asking about symptoms or changes you’ve noticed.
The main diagnostic test for ventricular arrhythmias is electrocardiography (often abbreviated as ECG or EKG). This test uses multiple sensors, called electrodes, which are placed on your chest. The electrodes detect your heart’s electrical activity — either while you’re resting or exercising — and display it as a wave pattern. Clinicians then review and analyze the wave patterns. An EKG usually takes just a few minutes and is done at a hospital or in a clinic or doctor's office.
In cases where an arrhythmia isn’t sustained and can’t be seen by an EKG, there are also devices that you can wear home to record arrhythmias that happen unpredictably. A clinician can review the data recorded after you return these devices.
Advertisement
Types of these devices include:
Depending on what causes a ventricular arrhythmia, it may be possible to cure it. However, if the cause is an underlying chronic condition or disease — especially a condition you’re born with — it’s usually not possible to cure it. When an arrhythmia isn’t curable, the goal becomes treating and managing it so it affects your life as little as possible.
The treatment for a ventricular arrhythmia depends on the type. Benign arrhythmias like PVCs don’t need treatment (unless they happen frequently and for longer periods). Other arrhythmias are treated long-term. Some are more dangerous and need emergency care.
Emergency treatments for ventricular arrhythmias include:
The following methods can treat ventricular arrhythmia in non-emergency situations:
What you can do to manage your ventricular arrhythmia strongly depends on your specific type of arrhythmia. In many cases, the most you can do is take your medication as instructed and see your doctor regularly as they recommend. You should also pay attention to your symptoms and report any changes to your doctor, especially if symptoms suddenly change or get worse.
Recovery time from ventricular arrhythmia depends on the type of arrhythmia and how it's treated. For arrhythmias treated with ablation or an ICD, you should recover from the procedure within days and feel better quickly. In the case of arrhythmias treated with medication, you should begin to notice changes within days or weeks.
The outlook for these arrhythmias greatly depends on which type you have and the underlying cause. Your healthcare provider is the best one to explain the outlook for your specific situation.
These kinds of arrhythmias usually aren’t preventable because they’re unpredictable. This is especially true when it comes to conditions that are inherited or present when you’re born.
However, it may be possible to delay or avoid developing conditions that can cause these arrhythmias. This generally includes doing the following:
Your healthcare provider can give you more information on things to watch for, especially indicators of future problems. In general, you should see your provider if you notice that your symptoms are changing or if they begin to affect your day-to-day life. You should also see a healthcare provider at least once a year for an annual physical, which can be a key way to catch health problems early.
You should go to the emergency room if you experience more serious symptoms related to ventricular arrhythmia. These include:
Ventricular arrhythmias can be very different from one person to the next. The best way to understand and manage your health is to see a healthcare provider if you think you might have a ventricular arrhythmia. You should also be sure to get an annual checkup or wellness exam. These yearly visits can be key to catching health problems early, which can make a big difference in preventing problems in the years to come.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
