Vasomotor (nonallergic) rhinitis is inflammation of nasal tissues that results in sneezing, nasal congestion, runny nose or postnasal drip. Unlike allergic rhinitis (or hay fever), the symptoms are of an unknown cause. Likely, they result from triggers that irritate your nose.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Vasomotor rhinitis happens when the tissues inside of your nose become inflamed (swollen). The inflammation causes unpleasant symptoms most people associate with allergies, like a stuffy or runny nose.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
However, unlike allergies (allergic rhinitis), vasomotor rhinitis doesn’t result from exposure to allergens, like pollen, mold, pet dander, etc. It’s not caused by viruses or bacteria either. Instead, you may experience symptoms because of weather changes, certain smells, eating, exercise, medications or other triggers that irritate your nose.
Vasomotor is also called idiopathic rhinitis. It’s a type of nonallergic rhinitis.
Anyone can develop vasomotor rhinitis, but most people get diagnosed after age 20. The majority of diagnoses occur between ages 30 and 60. It’s more common in women.
Allergic and nonallergic rhinitis (including vasomotor rhinitis) affects up to half of the population in industrialized countries. Vasomotor rhinitis accounts for anywhere from 15% to half of these cases.
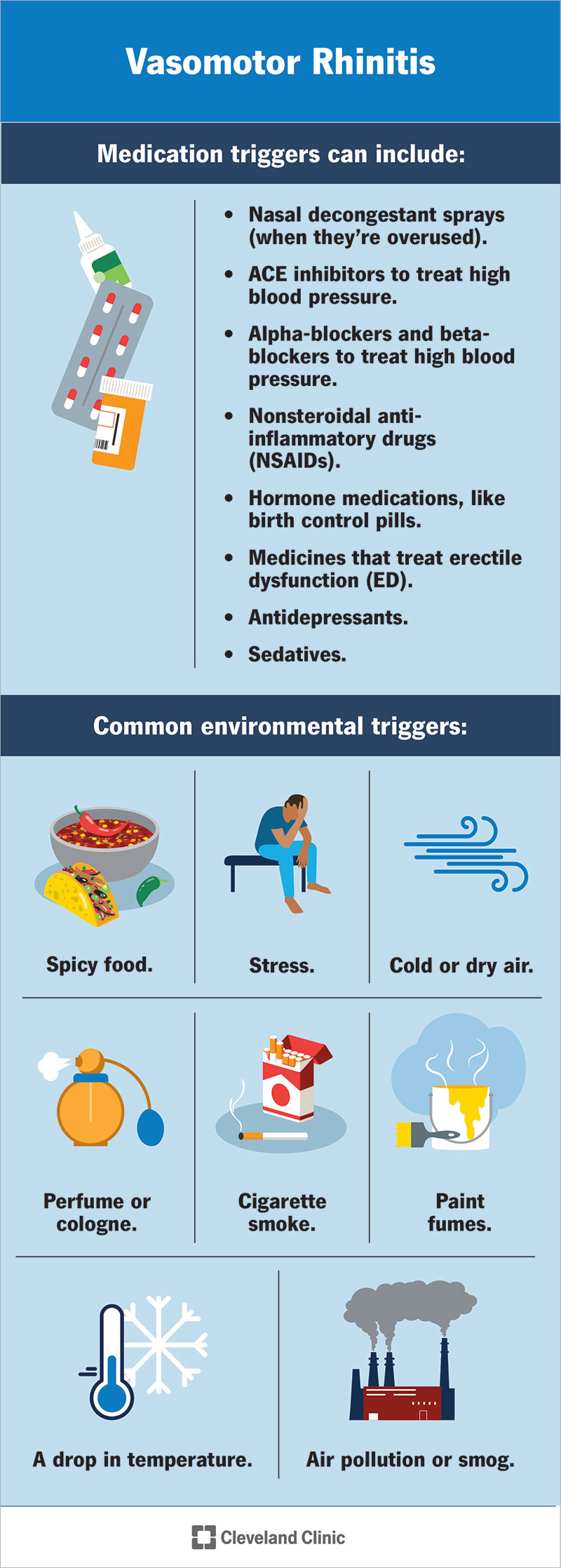
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17950-vasomotor-rhinitis)
Vasomotor rhinitis, unlike allergic rhinitis, doesn’t happen because you’re sensitive to a specific allergen, like tree pollen, dust mites or mold. Instead, various triggers may cause symptoms. It’s likely people with vasomotor rhinitis have heightened sensitivity to various substances and environmental changes that would trigger a response in most people — just in higher amounts.
If you have nasal inflammation and related symptoms resulting from an unknown cause, you might receive this diagnosis.
Advertisement
Triggers related to your environment, medicines you’re taking and even hormone changes can cause a reaction.
Your surroundings can trigger your senses and cause a reaction. Common environmental triggers include:
Certain medications can trigger nasal inflammation and swelling or make it worse. Triggers include:
Hormone changes can trigger a reaction. You may experience symptoms during times when hormones are in flux, including:
Nonallergic rhinitis may also result from using nonprescription drugs, like cocaine.
Unlike allergic rhinitis, symptoms of vasomotor rhinitis usually occur year-round. Instead of being seasonal — as is the case with seasonal allergies — symptoms flare up whenever you’re exposed to a trigger.
Symptoms of vasomotor rhinitis include:
Rarely, vasomotor rhinitis causes a foul-smelling crust to form inside your nose. The interior nasal tissues may bleed when you attempt to remove the crust.
No. It’s unrelated to germs that cause infections, like viruses and bacteria, which means you can’t catch it or spread it to someone else.
A healthcare provider can diagnose vasomotor rhinitis with a physical exam of your nose and throat and a review of your medical history. In some cases, further testing helps confirm your diagnosis.
Advertisement
There isn’t a cure for nonallergic rhinitis. Most people manage symptoms with self-care measures, changes to their environment and medicine.
If your condition results from exposure to triggers like perfumes, treatment may be as simple as avoiding the trigger. In those cases where avoiding the trigger is impossible, you can put measures in place to ease symptoms, try over-the-counter medications or get a prescription from a healthcare provider.
Using a humidifier at home or at work may ease symptoms. It may be helpful to rinse your nasal passages with a saline (salt water) solution to clean out your nose and nasal cavities (nasal irrigation).
Prescribed medications can decrease nasal inflammation and manage your symptoms. These medications may include:
Surgery may be an option if the medications aren’t helping or if another condition is intensifying the problem, like a deviated septum or nasal polyps.
Advertisement
Left untreated, vasomotor rhinitis may cause persistently blocked nasal passages or a constantly runny nose. These conditions can cause complications, including:
For many people, vasomotor rhinitis is a chronic, or long-term, condition. It may come and go over time.
There’s no way to prevent vasomotor rhinitis. You can lower your risk by avoiding triggers known to cause rhinitis.
If you have a runny nose, stuffy nose or postnasal drip that won’t go away, talk to a healthcare provider. They can help determine what’s triggering your symptoms. They can recommend treatments that can help.
The symptoms associated with vasomotor rhinitis — runny nose, nasal congestion and postnasal drip — are unpleasant, regardless of the cause. If you’re experiencing these symptoms, and they don’t improve, see a healthcare provider. They can determine whether the cause is related to allergies, an infection or something else (as is the case with vasomotor rhinitis). They can recommend or prescribe medicines that can help.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have conditions affecting your ears, nose and throat, you want experts you can trust. Cleveland Clinic’s otolaryngology specialists can help.
