ME/CFS is severe fatigue and exhaustion that lasts at least six months or longer. You might feel joint and muscle pain, headache and flu-like symptoms. Rest doesn’t help. It can prevent you from completing your daily routine or getting out of bed. Treatment options like medications, sleep habit changes or activity management may help.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a chronic illness that causes extreme tiredness that doesn’t improve with rest. It often gets worse after physical or mental activity. It can make daily tasks difficult. In some cases, even getting out of bed can feel impossible.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
With fatigue, symptoms feel like you have the flu. They can come and go, varying in intensity over time. Treatment options are available to manage ME/CFS.
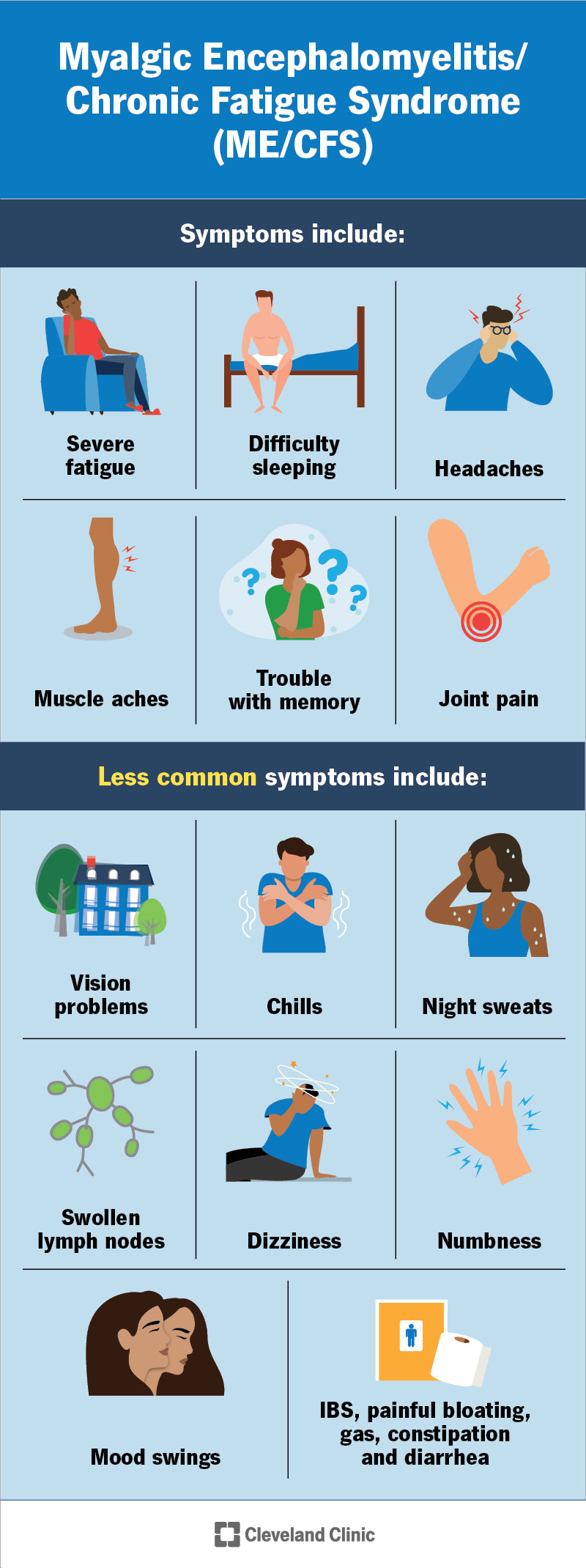
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17720-myalgic-encephalomyelitis-chronic-fatigue-syndrome-me-cfs)
ME/CFS symptoms include:
Other symptoms include:
Symptoms differ widely from person to person. They usually last for six months or longer. They may worsen after physical activity or mental effort. This is known as post-exertional malaise.
The exact cause of ME/CFS isn’t known. But studies show that these might be involved:
Advertisement
Research suggests the infections might trigger or cause a flare-up of symptoms:
Stress (physical or emotional) may also trigger symptoms.
While anyone can develop this condition, it’s more common among:
The fatigue from ME/CFS makes daily activities hard to do. Things like completing your routine or having the energy to get through the work or school day can be very difficult. You may need to make changes or ask for help to adjust to these symptoms.
ME/CFS can also lead to mental health challenges, like depression and anxiety. If you’re feeling down or overwhelmed, talk to a healthcare provider. There are treatments available that can help you feel better.
Healthcare providers diagnose ME/CFS after a physical exam, neurological exam and mental health evaluation. There’s no single test for ME/CFS. But lab tests, like blood or urine tests, can help rule out other conditions with similar symptoms.
The diagnostic criteria for ME/CFS, or the things that your physician will look for during an exam, include:
Getting a diagnosis can take time. Your doctor may need to run multiple tests, but not all at once. That process can be frustrating, especially when you’re already not feeling well. But try to stick with it. A clear diagnosis is the first step toward treatment that’s tailored to your body’s needs.
Treatment for ME/CFS may include:
If you have ME/CFS symptoms, contact a healthcare provider, especially if the symptoms last six months or more. They’ll evaluate your symptoms and create a treatment plan to help you feel better.
If you’re undergoing treatment, your doctor will schedule regular check-ins. This is to make sure treatment is working well and you don’t have any side effects. Let them know if you have any questions or concerns.
Advertisement
There’s no cure for ME/CFS. But your care team can help manage symptoms with treatments that fit your lifestyle. While many people see improvement, some may not return to their previous level of health or activity. The condition affects everyone differently.
Making routine changes isn’t easy, and sticking with them can be tough. Your physician may recommend cognitive behavioral therapy (CBT) to help you cope and support your mental well-being as you adjust.
Life expectancy with ME/CFS can vary. Some people live a typical lifespan, while others may have a shorter one. Research suggests a higher risk of suicide, often linked to mental health challenges.
If you have concerns about your future, talk to your physician. They can give you the most up-to-date information on your case.
Living with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) can feel like you’re carrying around a weight all day. You’re constantly exhausted. And even after rest, you still don’t wake up feeling refreshed.
If this sounds familiar, talk to a healthcare provider. There are treatments that can help you manage symptoms. Finding what works best might take time, but don’t give up. Some days may be harder than others, and that’s OK. What matters is knowing that support and tools are out there, and they can make a real difference.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
