Chronic traumatic encephalopathy (CTE) is a degenerative brain condition that happens after repeated head injuries. CTE usually affects athletes who play contact sports or military personnel. There’s no cure for CTE, but your healthcare provider will suggest treatments to help you manage the symptoms you experience.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
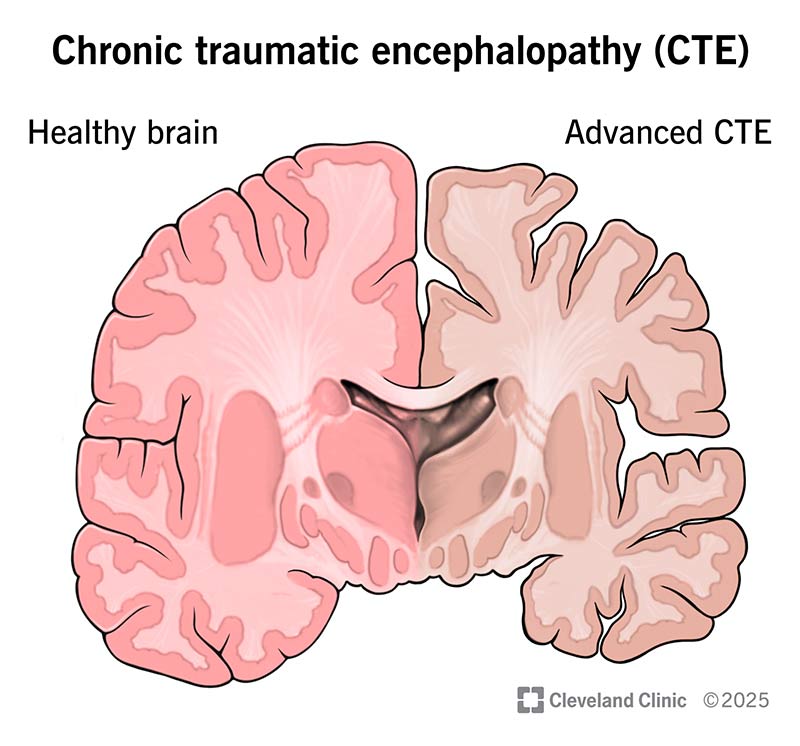
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/chronic-traumatic-encephalopathy)
Chronic traumatic encephalopathy (CTE) is a brain condition that can develop if you experience repeated impacts or blows to your head.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
CTE permanently destroys nerve cells in your brain. This is called neurodegeneration. Over time, this damage can cause changes in your behavior and mental abilities.
Visit a healthcare provider if you think you’ve experienced a head injury, especially if you know this isn’t your first one. They’ll help you understand how you can protect your brain from more damage.
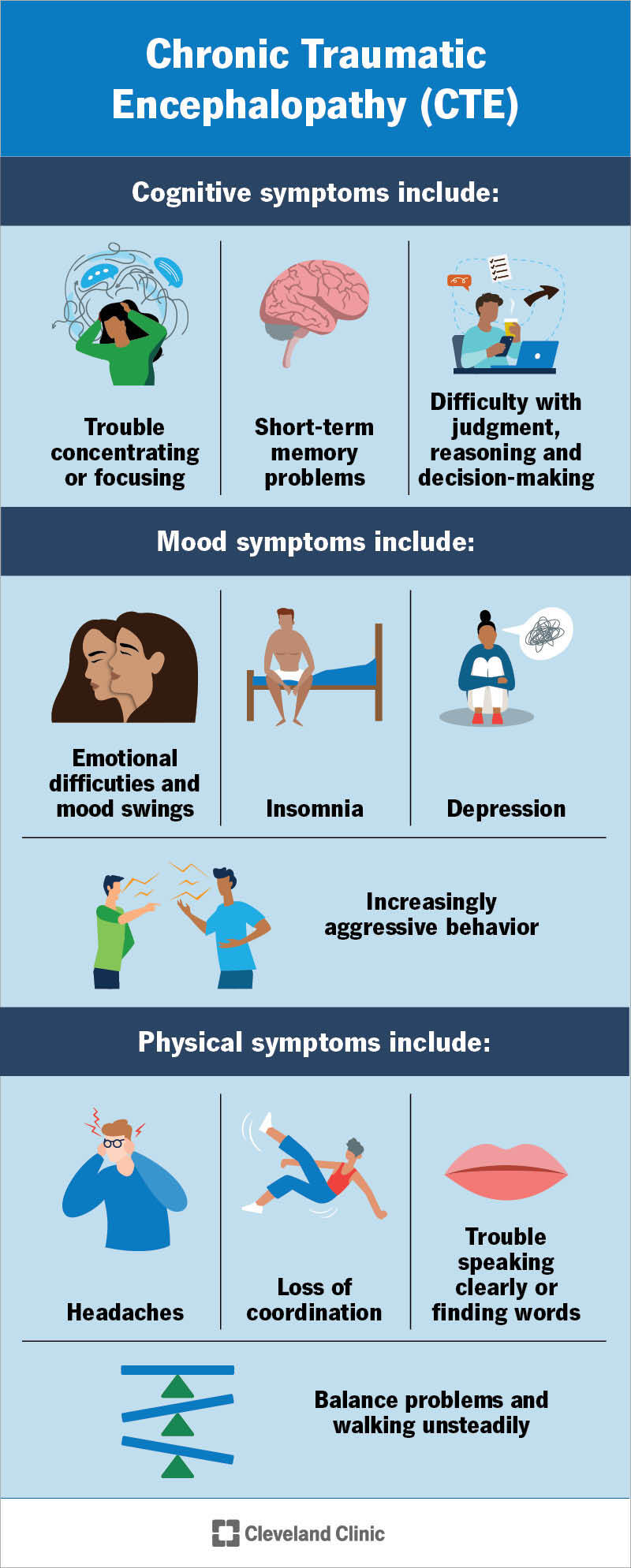
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/chronic-traumatic-encephalopathy-01)
CTE shares symptoms with other brain conditions that cause neurodegeneration. It can affect:
CTE can affect certain mental abilities. You might notice:
Neurodegeneration can affect the parts of your brain that control your personality and emotions. You might experience:
It might be hard to notice some of these changes in yourself. Loved ones might tell you you’re acting differently or “not like yourself.” Try to remember that people care about you and are sharing these concerns because they want to make sure you’re feeling safe and healthy.
Advertisement
CTE can affect your brain’s ability to control your body. Some symptoms can include:
Experiencing repeated head injuries causes CTE. Experts are still studying exactly why it happens in some people but not others. But they know having multiple head injuries is one of the most common causes. People with chronic traumatic encephalopathy almost always have a history of repeated head injuries over many years.
You don’t have to pass out (get “knocked out”) for a hit to your head to damage your brain. The effects of repeated head impacts build up over time.
Researchers think a buildup of abnormal tau proteins in your brain may also cause CTE. Tau proteins help your cells keep their shape. But if repeated head hits damage your cells, the tau proteins may lose their normal structure.
Having multiple head injuries is the biggest risk factor for CTE. Some activities that increase your risk include:
Some experts think having certain genes may increase your CTE risk. Researchers are still studying these potential genetic factors.
How to lower your risk for CTE
Avoiding head injuries is the only way to lower your risk of developing CTE. Wear the right protective equipment for all activities and sports, especially helmets or protective headwear.
There’s no way to diagnose chronic traumatic encephalopathy in a living person. The only way healthcare providers can confirm CTE is by examining samples of a person’s brain with a microscope. But they can only do this during an autopsy after someone dies.
Even though your provider can’t definitively diagnose CTE while you’re alive, they can still make an educated assumption. They’ll build a diagnosis using a few factors:
Experiencing CTE symptoms doesn’t automatically mean you have it. Lots of other conditions can cause similar symptoms. Your provider will use tests to help diagnose or rule out these other issues. You might need:
Your healthcare provider can’t directly treat CTE, and there’s no way to reverse the brain damage. Instead, they’ll suggest ways to manage any symptoms you’re experiencing. You might need:
Advertisement
Experts are still researching CTE. Ask your provider about any clinical trials that you might be eligible for. These may let you try new or experimental treatments.
Visit a healthcare provider if you think you have a head injury. Tell them how many head injuries you’ve had (if you can remember them all or know they happened).
It might help to ask your provider a few questions, including:
In the U.S., you can call the 988 Suicide & Crisis Lifeline if you’re thinking about hurting yourself or have suicidal thoughts. Call or text 988 anytime for 24/7 help from specially trained providers and counselors.
CTE is a permanent, lifelong condition. It’s also progressive, which means the symptoms will get worse over time. These changes can happen slowly (over years or even decades).
Chronic traumatic encephalopathy isn’t fatal. It won’t affect your life expectancy. But as it progresses, it can cause complications that affect your health and well-being. At the end stage of CTE, you might lose the ability to feed, bathe or dress yourself.
Advertisement
You can start planning for the future before you experience more severe symptoms. You might want to think about things like advance directives and legal and financial plans.
Your healthcare provider will help you understand what you and your loved ones can expect.
Chronic traumatic encephalopathy (CTE) can be a confusing condition. It might be hard to understand how it can have such a big impact on your health and life if providers can’t confirm you have it. But it’s real and so are the symptoms it causes.
Talk to your healthcare provider or a mental health professional if you feel like you need extra support. They’ll make sure you feel safe and confident as you learn to live with CTE and any changes it brings.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Traumatic brain injuries can be serious or life-threatening. Cleveland Clinic’s experts provide fast treatment to give you the best chance of recovery.
