Pulmonary alveolar proteinosis (PAP) is a rare lung disease that leads to clogged air sacs (alveoli) in your lungs. It can cause breathing problems, low blood oxygen levels and other problems.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
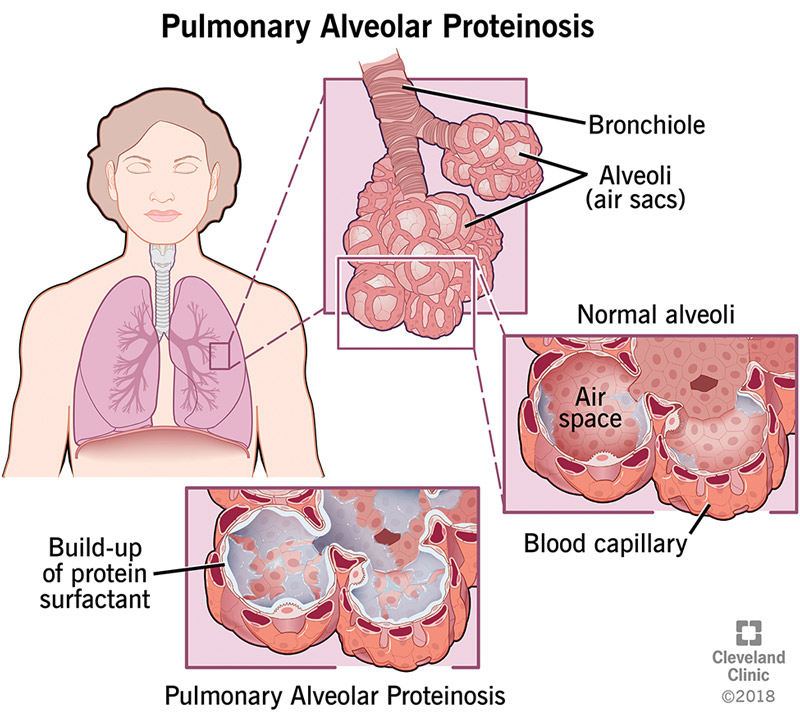
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17398-pulmonary-alveolar-proteinosis-pap)
Pulmonary alveolar proteinosis (PAP) is a rare lung disease caused by a buildup of proteins, fats and other substances in the air sacs of your lungs (alveoli). It prevents air from getting through the alveoli, so your blood doesn’t get enough oxygen. PAP can make it difficult to breathe.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
PAP is a serious lung condition, and getting this diagnosis can be scary. But you can manage the disease and its symptoms with the right treatment. If you have PAP, getting care from an experienced pulmonary medicine doctor (healthcare provider specializing in lung diseases) is important. Your provider can also advise you on healthy lifestyle changes that can improve your quality of life.
The different types of PAP include:
Autoimmune and secondary PAP usually affect people between the ages of 30 and 60. These two types are more common in males. Smoking and exposure to certain dusts or chemicals increase your risk. Congenital PAP is most common in children under the age of 10, but it may start to appear at any age.
Advertisement
PAP is rare. It affects between 3 and 40 people per million worldwide.
The alveoli have thin walls that allow oxygen to pass from your lungs into your blood. The walls naturally have an oily layer of proteins and fats (called surfactants) that help them stay open so oxygen can pass through. Cells called alveolar macrophages periodically clean the surfactants from the air sacs so they don’t get clogged.
But if you have PAP, the macrophages don’t receive the signal they need to clean your alveolar walls. So surfactants build up and block your alveoli. Oxygen can’t pass through to your blood as it should.
Shortness of breath (dyspnea) is the most common symptom of PAP. Most people with the disease have difficulty breathing while exercising, but some also have breathing problems at rest.
Other symptoms of PAP include:
PAP can cause life-threatening respiratory failure in severe cases. The disease’s course, however, can range from spontaneous remission to stability, or death due to respiratory failure or secondary infections.
Your healthcare provider does a physical exam and listens to your lungs if they suspect you have PAP. They’ll also ask questions about your personal and family medical history, as well as your lifestyle. Be sure to tell your provider if you smoke or have had exposure to dust, chemicals or other toxins.
Tests for PAP may include:
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_uti3jdrz/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Lung Washing (Lung Lavage) for Pulmonary Alveolar Proteinosis (PAP).
There isn’t a cure for pulmonary alveolar proteinosis at this time.
The most common treatment for PAP is whole-lung lavage (WLL), also called “lung washing.” A healthcare provider uses a bronchoscope and saline (sterilized salt water) to clean one lung at a time so you can breathe easier. The procedure takes between four and five hours. You may need the procedure every few months or every year, depending on the severity of your symptoms. Treatment varies depending on the severity of the disease. Some people with PAP won’t need WLL due to the varying course of the disease.
During whole-lung lavage:
Advertisement
Other treatments may include:
Regular treatments such as whole-lung lavage can help you breathe better and relieve other symptoms. PAP clears up on its own in a small number of people. Without treatment, severe PAP can sometimes cause respiratory failure or death.
Advertisement
There are different types of pulmonary alveolar proteinosis. It’s not possible to prevent autoimmune-related or congenital PAP. But avoiding toxins — or wearing a respirator or a well-fitted facemask if you can’t avoid them — may help prevent secondary PAP. Make sure that your facemask covers your mouth and nose.
Pulmonary alveolar proteinosis (PAP) is a rare lung disease that clogs the air sacs in your lungs. It can cause breathing problems and a range of other symptoms. Several effective therapies manage the effects of PAP. If you have this condition, seek treatment from a multispecialty team of healthcare providers. They can work together to help improve your quality of life.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Breathing issues can affect your life in many ways. Cleveland Clinic’s respiratory therapy program treats your symptoms so you can feel better day to day.
