Inclusion body myositis is an inflammatory and degenerative muscle disease. It features abnormal protein deposits called inclusion bodies that cluster inside your muscle cells and contribute to weakening them. Over time, you’ll notice your limbs growing increasingly weaker, and you may develop difficulties with ordinary tasks.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
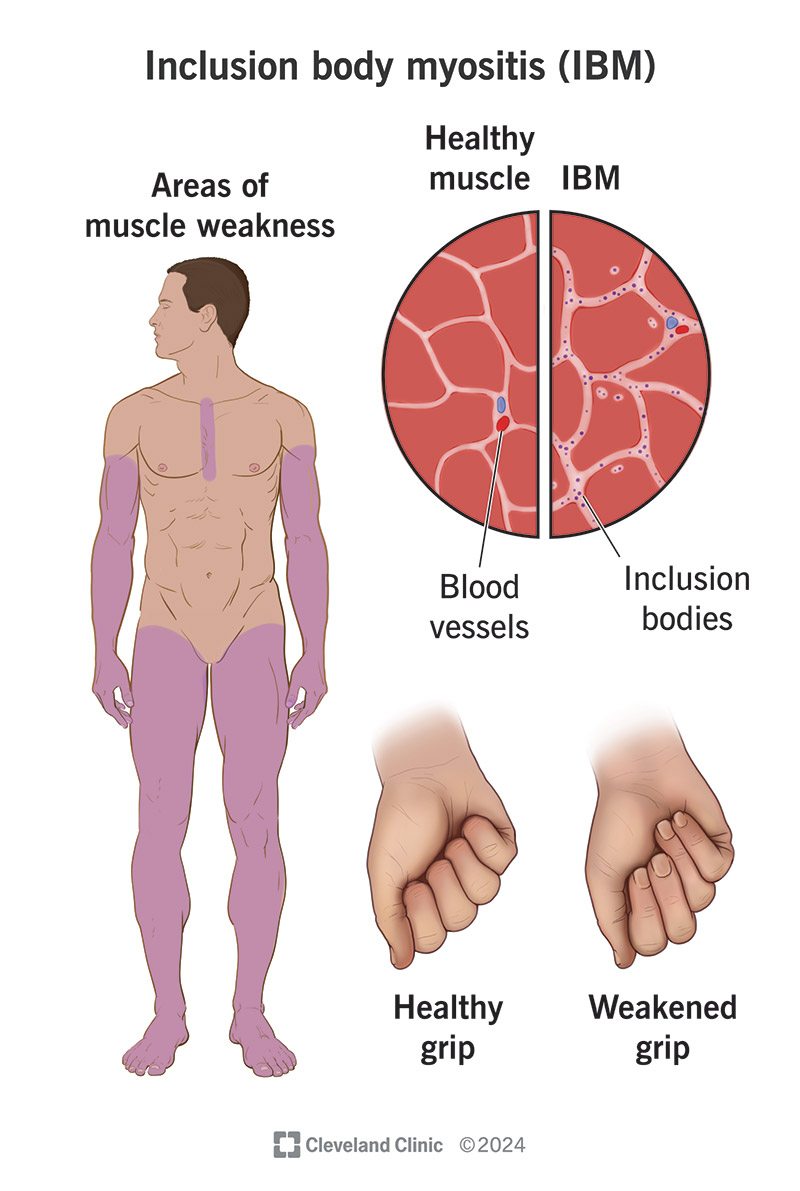
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/inclusion-body-myositis.jpg)
Inclusion body myositis (IBM) is a degenerative muscle disease that causes gradual and painless weakening of your muscles. Symptoms usually appear after the age of 50. You might notice that you start to have trouble pinching and grasping objects, or that you’ve started tripping and falling a lot.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
IBM progresses over several years. It isn’t life-threatening, but it can become disabling over time. It may affect one side of your body more than the other. Up to half of people develop swallowing difficulties. There’s no cure, but physical therapy can help you preserve as much of your mobility as possible.
Inclusion body myositis is one of the most common myopathies — diseases that attack and weaken your muscle fibers. Research suggests IBM may affect between 5 and 9 out of every 1 million adults. It’s more common in men than women people by a ratio of 3:1.
Muscle weakness from IBM occurs gradually and usually begins in your limbs. You might notice it in your lower body (legs and feet) or upper body (arms, wrists and fingers) first. Some people notice a lack of dexterity when they try to button their shirts or write with pens. Others might start tripping and falling.
As symptoms progress, you might notice:
Advertisement
Inclusion body myositis is idiopathic, which means that it appears to happen spontaneously. As with other types of myositis, chronic inflammation in your muscles contributes to weakening them. But researchers don’t know what causes the inflammation. It might be a type of autoimmune disease.
Inclusion bodies also play a part in IBM. These are clumps of abnormal proteins within your muscle cells. They may be byproducts of a viral infection, cellular damage or genetic mutations. Inclusion bodies often occur in neurodegenerative diseases, like ALS. They may interfere with how your cells function.
Inclusion body myositis sometimes goes by the more specific name of “sporadic inclusion body myositis (sIBM).” Sporadic means random. This is to distinguish it from similar conditions that are hereditary, called “hereditary inclusion body myopathies (hIMB).” Inclusion body myopathies include both types.
To diagnose IBM, a healthcare provider will begin by reviewing your symptoms and examining your muscles. Symptoms of inclusion body myositis may resemble many other related conditions, including polymyositis and myasthenia gravis. Your provider will look for distinguishing features, like:
They may run a few lab tests to rule out other conditions, like:
The definitive way to diagnose inclusion-body myositis is to take a tissue sample (biopsy) from one of your affected muscles. A pathologist will examine the tissue under a microscope. If you have IBM, they’ll see inclusion bodies in the sample — clumps of abnormal proteins inside bubble-like spaces (vacuoles).
There’s no effective course of treatment for inclusion body myositis. Unlike other inflammatory and autoimmune conditions, it doesn’t respond to corticosteroids or immunosuppressant drugs. But physical therapy and regular exercise are crucial to preserving your muscle strength as much as possible.
Advertisement
When the disease becomes more advanced and disabling, you may need to learn new ways of doing things. This is where occupational therapy can help. Some people might need to learn how to operate a wheelchair. If you develop swallowing difficulties, a speech-language pathologist (SLP) might be able to help.
If you have IBM, it’ll continue to slowly progress. It won’t affect your life expectancy, but it’ll affect your quality of life. You may need to learn to rely on others more or learn new ways of doing things. Most people don’t lose the ability to walk, but some may need a wheelchair after 10 to 15 years.
You’ll likely be living a long time with inclusion body myositis, and it’ll gradually become more challenging. The best way forward is to adopt a long-term plan to take care of your physical and mental health. That means keeping up with the many small habits that keep you feeling your best. For instance:
Advertisement
Inclusion body myositis seems to come out of nowhere, usually in the latter half of your life. No one expects to suddenly develop a degenerative disease with no known cure. It can be a lot to process and to explain to those who care about you, especially when they’ve likely never heard of the disease.
But this is a slow-progressing disease, and there’s plenty of time to anticipate the changes ahead and make adjustments. No one can say for certain how it’ll play out for you. But with an optimistic approach, there’s a lot you can do to maintain your overall health and well-being in the years to come.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have an inflammatory or autoimmune condition, you need experts by your side. At Cleveland Clinic, we’ll create an individualized treatment plan for you.
