Impetigo is a common skin infection that most often affects young children. Bacteria including Staphylococcus aureus (S. aureus or “staph”) and Group A streptococcus (“strep”) cause the infection, which can lead to itchy sores and blisters. Treatment includes antibiotics. Within a few days of treatment, your child should start to feel better.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
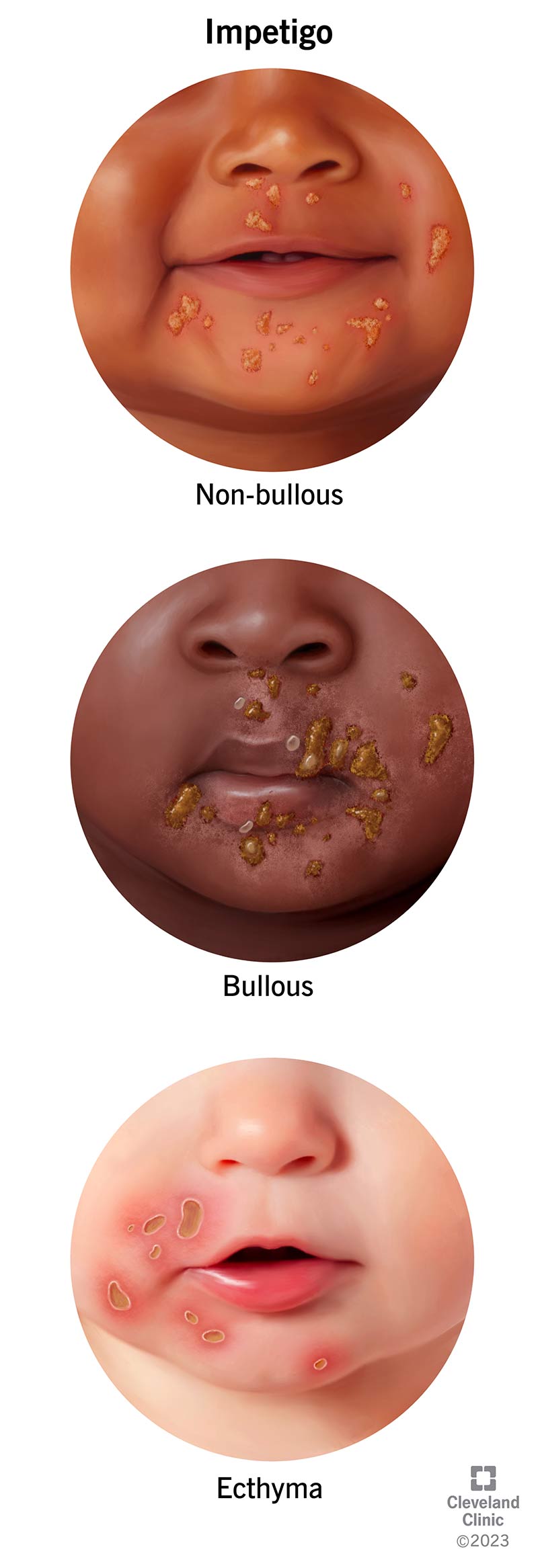
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15134-impetigo)
Impetigo (pronounced “im-peh-TIE-go”) is an itchy, sometimes painful, skin infection. When your child gets a cut, bite or scratch that opens their skin, bacteria can enter and cause a bacterial infection. But impetigo can infect skin even if it’s not broken or punctured.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Impetigo happens more often in warmer months when children are outside. Typically, the first signs of impetigo are sores and blisters on your child’s mouth and nose. It can also appear on your child’s scalp, hairline, legs and arms.
There are a few different types of impetigo, including non-bullous, bullous and ecthyma.
Non-bullous is early-stage impetigo. It’s the most common type. The non-bullous impetigo early stages include:
Bullous impetigo is a rarer type of skin infection. It’s more common in infants. More than 90% of cases of bullous impetigo affect children younger than age 2. The stages of this type include:
Untreated impetigo can develop into ecthyma. Ecthyma is a more serious type of skin infection. It goes deeper into your child’s skin. The stages typically include:
Advertisement
Impetigo is the most common skin infection in kids between the ages of 2 and 5. Older children can also get it. It accounts for about 10% of skin conditions in children.
Yes, impetigo can affect adults. In adults, the condition may occur after another skin issue. Sometimes it develops after you’ve had a cold or another virus. You may be at higher risk if you:
Impetigo and cold sores are both common skin infections that can cause blisters. Cold sores usually occur around your mouth and consist of small blisters. Impetigo can form around your mouth but also on other parts of your face and body. It causes larger blisters. A bacteria causes impetigo, whereas cold sores are a symptom of the herpes simplex virus (HSV).
Impetigo and weeping eczema are both common skin conditions. Impetigo is a type of skin infection, whereas eczema is a type of dermatitis. Impetigo causes crusty, honey-colored sores and blisters. Weeping eczema sometimes causes blisters with clear or straw-colored fluid. The blisters may be purple or red and they can ooze or “weep” the fluid.
Typically, symptoms of impetigo develop within three days once the bacteria infect your child’s skin. Impetigo on the face starts around the mouth and nose. However, impetigo on the scalp or hairline can also occur.
Impetigo includes blisters, rashes and other skin wounds (lesions). The condition includes the following characteristics:
If you or your child has impetigo caused by Staph bacteria, you may notice:
Advertisement
Impetigo causes include certain types of bacteria that lead to infection. The most common impetigo bacteria include:
The bacteria usually enter your child’s skin through a cut, scrape, rash or insect bite. After they enter your child’s body, the bacteria continue growing in their skin. This can lead to inflammation and infection in the top layers of your child’s skin.
Your child may also get impetigo by scratching something itchy on their skin, such as chickenpox or eczema. When they scratch, it breaks the skin, making it easy for bacteria to get in.
Impetigo may also occur without any skin breakage. Instead, it can occur after you’ve experienced another skin condition, such as:
Adults can also get impetigo through health conditions such as tattoo infections.
No, stress doesn’t cause impetigo. However, stress can weaken your immune system. With a weakened immune system, it’s easier for bacteria to infect you and harder for your body to fight them.
Impetigo is highly contagious. Most people get it through direct skin-to-skin contact. You can get impetigo by coming into contact with sores, mucus or nasal discharge from someone who has it. Children and athletes, such as football players and wrestlers, often get it this way.
Advertisement
People can also spread impetigo by sharing items such as towels, clothing or other personal items with an infected person.
Without treatment, impetigo can be contagious for weeks. After starting impetigo treatment, the condition is contagious until:
Complications are rare. Certain strains of strep bacteria that cause impetigo can also cause glomerulonephritis. This inflammatory kidney disease can produce high blood pressure and blood in your pee (hematuria). Other complications of impetigo may include:
A healthcare provider will diagnose impetigo based on how your child’s sores look. They may take a skin culture to send to a laboratory. This will help your provider determine the right antibiotic to prescribe your child.
Impetigo treatment includes antibiotics. A provider may prescribe topical antibiotics to put directly on your child’s skin. Impetigo treatments may also include an oral antibiotic (a liquid or pill taken by mouth) if the impetigo covers a large area of your child’s skin or multiple body parts.
Advertisement
Impetigo medication may include:
Impetigo won’t go away for everyone in 24 hours. However, some studies have shown that the condition goes away quicker when you use an antibiotic cream. Providers recommend these creams to help the symptoms go away fast and to help stop the infection from spreading. Therefore, the sooner you receive treatment, the better.
You’ll need prescription antibiotic medication to treat most forms of impetigo. For minor skin infections that haven’t spread, you can try treating the area with an over-the-counter (OTC) antibiotic cream or ointment that contains bacitracin. Then, place a nonstick bandage over the area to help prevent the infection from spreading.
Taking care of your child’s skin can help clear up an impetigo infection faster. Skincare steps you can take to get rid of an impetigo infection quickly include:
Impetigo may go away on its own in a few weeks. Still, healthcare providers recommend treating it for several reasons:
Antibiotics can treat impetigo, but the condition can return, especially in young children. Children are especially prone to scratching and opening their scabs, putting them at a higher risk of re-infection. However, most kids recover with no complications after they receive treatment.
With treatment, your child usually isn’t contagious after 48 hours. The sores may take some time to heal completely, but the infection rarely leaves scars.
Without treatment, impetigo may clear up on its own in a few weeks. But there’s a greater risk of developing complications and you may see new sores and blisters.
The bacteria that cause impetigo can live on dry surfaces for weeks or even months.
Impetigo is very contagious. Your child should stay home from school for 48 hours after starting an antibiotic. Adults don’t need to stay home from work, but they should avoid contact with other people and keep their sores and blisters covered.
The best ways to prevent infections include:
If your healthcare provider diagnosed you or your child with impetigo, these treatment tips can help:
Impetigo is a common skin condition that usually affects young children. Impetigo is very contagious, so keep your child home until they’ve had at least two days of antibiotics. The medicine will clear up the rash. To prevent impetigo, practice good hygiene. Clean and cover any cuts or scratches to keep them from getting infected.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
As your child grows, you need healthcare providers by your side to guide you through each step. Cleveland Clinic Children’s is there with care you can trust.
