A TB test checks to see if you’ve been infected with tuberculosis (TB). There are two types of TB tests: a skin test and a blood test. TB skin and blood tests can show if you’ve ever been exposed to the bacterium that causes TB, but they can’t determine if you have a latent (dormant) or active TB infection.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
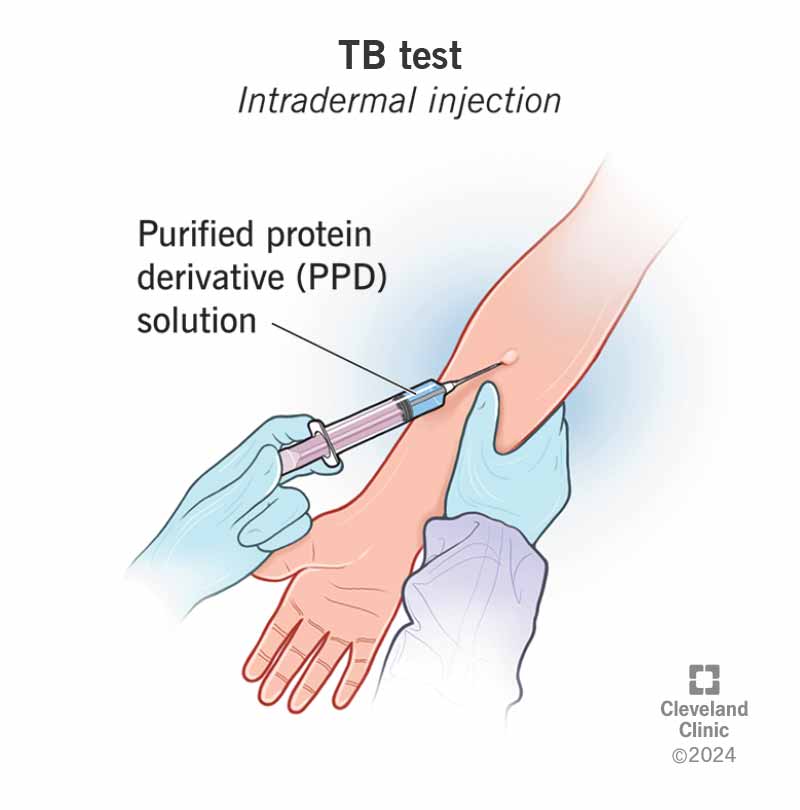
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22751-tuberculosis)
A TB test checks to see if you’ve been infected with Mycobacterium tuberculosis complex, which is the bacteria that causes tuberculosis (TB). There are two types of latent tuberculosis infection (LTBI) screen tests: a skin test and a blood test.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A TB skin test is also called a Mantoux test or tuberculin skin test (TST). A TB blood test is also called an Interferon-Gamma Release Assay (IGRA). TB skin tests are more common and are the preferred type for children under age 5. But blood tests for TB are becoming more common, especially for healthcare workers and those who have compromised immune systems or are going to become immunocompromised by medications.
TB skin and blood tests can show if you’ve ever been infected with M. tuberculosis complex, but they can’t distinguish between a latent (dormant) or active TB infection. You’ll need additional tests (like a sputum test) to see if you have an active infection.
You may need a TB test if you have symptoms of an active TB infection or if you’re at a higher risk for getting TB. In addition, some childcare centers, hospitals and other facilities require you to be tested for TB to work there.
You may be at a higher risk for getting TB if you:
Advertisement
It depends on if you have risk factors for tuberculosis infection. If you’re at a higher risk for TB, your healthcare provider may recommend yearly TB testing. If your risk for tuberculosis infection is low, you can go several years without getting a TB test. Ask your healthcare provider what frequency they recommend based on your specific situation.
Both types of TB tests — the skin test and blood test — work by measuring your immune system’s response to antigens taken from the bacterium that causes TB: Mycobacterium tuberculosis. An antigen is any substance that causes your immune system to produce a response against it. This means your immune system doesn’t recognize the substance and is trying to fight it off.
A TB skin test measures your immune system’s response to a purified protein derivative (PPD) solution injected under your skin. PPD is a protein that comes from Mycobacterium tuberculosis.
It’s not live bacteria, and it won’t make you sick. If you’ve ever been exposed to the TB bacteria, your skin will react to the antigens by developing a firm, red bump at the site of the injection within three days.
In most cases, if you’ve been infected with TB, certain white blood cells from your blood sample will release a protein called interferon-gamma (IFN- γ) when mixed with antigens derived from Mycobacterium tuberculosis in a laboratory.
To conduct the tests, laboratory scientists mix your blood sample with antigens and controls and measure the reaction using a method called immunoassay. They’ll interpret your results as negative, positive or indeterminate.
The TB testing process is different based on what kind you get — the skin test or the blood test.
A TB skin test requires two or three visits with a healthcare provider. During the first visit, they inject fluid into your forearm. On the second and third visits, the healthcare provider assesses your skin’s reaction to the injection.
During the first visit, you can expect:
You’ll then return to your provider within 48 to 72 hours so that they can look for a reaction on your forearm where they injected the fluid. Firm swelling and redness at the site may indicate a TB infection. It’s important to go to your second appointment to get an official result. If you don’t return within 72 hours, you’ll need to take the test again. People with weak immune systems and those with frail skin conditions may not have reliable skin test results.
Advertisement
You can expect to experience the following during a blood test:
The entire procedure usually takes less than five minutes.
After a healthcare provider has collected your blood sample, they’ll send it to a laboratory for testing. Once the test results are back, your healthcare provider will share the results with you.
For both a TB skin test and blood test, you may feel a small pinch from the needle, but this will be brief. For a skin TB test, the liquid the healthcare provider injects shouldn’t burn or feel uncomfortable.
There are very few side effects of having a TB skin test or blood test.
Advertisement
For a TB skin test, you may feel a pinch when you get the injection. Some people report discoloration, swelling and tenderness at the injection site.
For a TB blood test, you may have slight tenderness or a bruise at the site of the blood draw, but this usually resolves quickly.
The results of a TB skin test or blood test will be either negative or positive. It’s important to remember that these tests only show if you’ve been exposed to the tuberculosis infection — not if your infection is active or latent. You might have a false-positive skin test result if you’ve received a TB vaccine (BCG).
If your TB skin test or blood test is positive, it probably means you’ve been exposed to the bacterium that causes TB. Your healthcare provider will likely order more tests to help make a diagnosis. Tests that diagnose active TB infections include chest X-rays and laboratory tests on a sputum sample. Sputum is the thick mucus that you cough up from your lungs. It’s different from spit or saliva. You’ll need treatment for TB, whether it’s latent or active.
If your TB skin or blood test is negative, you likely haven’t been exposed to the TB bacterium. A negative TB skin test means your skin didn’t react to the liquid. You may need further testing if your results were negative, but you have symptoms of TB.
Advertisement
It takes 48 to 72 hours to complete a skin TB test. Once you have your second visit with your healthcare provider, they’ll be able to tell you whether your skin’s reaction indicates that you have a TB infection.
In most cases, you should get the results of your TB blood test within one to two days, though it could take longer.
A positive TB skin test will look like a firm, red bump. Your provider will measure the size of the firmness of the bump. Your provider considers your particular risk factors to determine the results of your test. You’re considered positive if your bump is:
Even if you think you know the result of your test based on your skin’s appearance 48 to 72 hours after you were first injected with the liquid, it’s important to see your healthcare provider for the second visit to get a proper assessment. They’re specially trained to observe your skin for a reaction and need to document your result.
If you have symptoms of TB — like a persistent cough, chest pain and fever — or think you’ve been exposed to someone with an active TB infection, it’s important to see your provider as soon as possible.
TB can be deadly if it’s not properly treated. Most cases of TB can be cured if you take antibiotics as directed by your healthcare provider. Both active and latent TB should be treated, but the type and medications and how long you need them are different if you have active versus latent TB.
TB testing and screening are essential for public health. Since TB can be deadly and spreads from person to person easily, it’s important to get tested if you have symptoms, are at high risk for developing active TB, or you’re at high risk of being exposed to the infection. Once you know your results, your healthcare provider will let you know if you need to undergo further tests. Don’t be afraid to ask your provider questions. They’re here to help you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
