Rheumatic fever is an autoimmune condition that inflames your child’s tissues, such as their joints and heart. Another name for the disease is acute rheumatic fever. It occurs when your child’s immune system overreacts to an untreated strep throat or scarlet fever infection. One of the most common symptoms of the disease is a red, jagged rash.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Rheumatic fever is a rare autoimmune disease that causes inflammation of your child’s tissues and organs. Healthcare providers also call it acute rheumatic fever. The condition occurs when your child’s immune system overreacts to an untreated strep throat or scarlet fever infection.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Strep throat and scarlet fever are both bacterial infections caused by group A Streptococcus. If your child doesn’t receive treatment for these infections, their immune system may attack its own tissues. This can cause swelling and inflammation that may affect your child’s joints, heart and blood vessels.
Scarlet fever and strep throat are group A Streptococcus infections. A type of bacteria called group A Streptococcus causes both infections. Healthcare providers treat them with antibiotics.
Rheumatic fever is a very rare complication of scarlet fever and strep throat. It can happen when one of these infections goes untreated.
While strep infections are common in the United States, rheumatic fever isn’t. Because antibiotics are widely available in the U.S., most people get treatment for strep throat and scarlet fever. Clearing up these conditions prevents rheumatic fever.
Rheumatic fever happens more often in places with limited resources, such as resource-poor countries. But it can occur in the U.S., especially in areas with limited access to medical care.
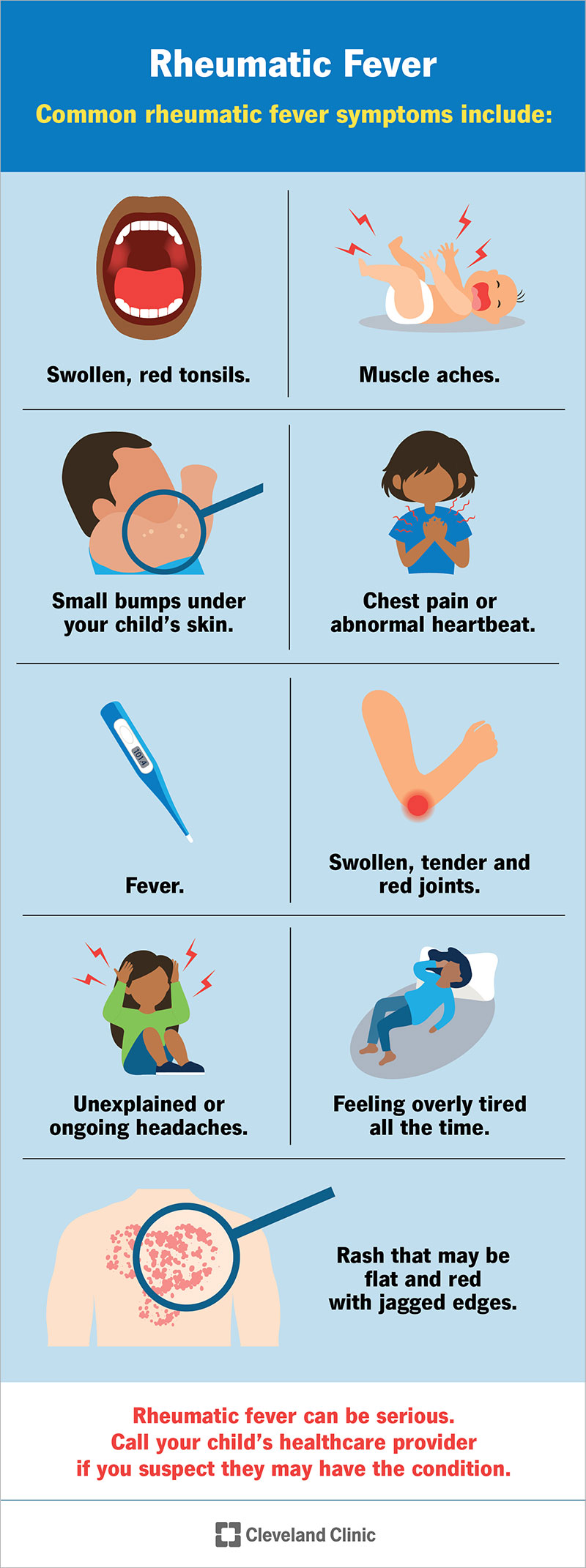
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16616-rheumatic-fever)
Rheumatic fever can affect people in different ways. Sometimes, people have such mild strep they don’t realize they had an infection until rheumatic fever develops later on.
Advertisement
Rheumatic fever causes many symptoms that look similar to other health issues. Most of these other conditions are routine and not dangerous. Symptoms can vary widely depending on what part of your child’s body the disease impacts. Because rheumatic fever can be serious, always call your child’s healthcare provider if you suspect they may have the condition.
One common symptom of rheumatic fever is a rash. The rash may be flat and red with irregular edges. Other common rheumatic fever symptoms include:
Rheumatic fever is an overreaction of your child’s immune system that causes it to fight healthy tissues. An untreated strep throat or scarlet fever infection can trigger this overreaction. It happens when your child doesn’t receive antibiotic treatment for group A Streptococcus infections.
When your body’s defenses (antibodies) begin to fight back, the reaction can damage healthy tissues and organs instead of the bacteria.
Anyone can get rheumatic fever. But it mostly affects children and teenagers (ages 5 to 15). Rheumatic fever usually develops two to three weeks after an untreated strep throat or scarlet fever infection. Rheumatic fever generally doesn’t occur in children younger than 5 and older than 15.
Most people who get strep throat or scarlet fever don’t develop rheumatic fever. It only happens when children don’t receive treatment for the infections. Even then, rheumatic fever is exceedingly rare in the U.S.
Certain factors can increase your risk of getting rheumatic fever:
Advertisement
It’s very rare, but adults can also get rheumatic fever.
Rheumatic fever isn’t contagious. You can’t give it to or get it from someone else. But strep throat and scarlet fever are contagious. These infections spread through respiratory droplets (by coughing or sneezing on someone else).
Rheumatic fever doesn’t always affect the heart. But when it does, it can damage heart tissues, especially the heart valves. Scarred heart tissue doesn’t work correctly. Over time, rheumatic fever may lead to permanent heart damage. Providers may call this condition rheumatic heart disease or congestive heart failure.
If rheumatic fever injures a heart valve, your child’s provider may recommend surgery to repair or replace the affected valve. Heart damage may show up 10 to 20 years after a rheumatic fever diagnosis. It’s important to stay in regular contact with a healthcare provider you trust.
Rheumatic fever has similar early symptoms to rheumatoid arthritis (RA), but the two conditions aren’t related. Both conditions may affect your child’s joints, but rheumatic fever usually lasts only a few weeks, whereas RA is a lifelong disorder. Children under age 16 are diagnosed with juvenile idiopathic arthritis, not rheumatoid arthritis.
Advertisement
If your child has had a sore throat for more than a couple of days, reach out to their healthcare provider. Treating a group A streptococcal infection can prevent rheumatic fever.
If their provider suspects rheumatic fever, they’ll first swab your child’s throat to check for group A Streptococcus bacteria. They may use a rapid strep test or order a throat culture.
A rapid strep test can provide results within 10 minutes. A throat culture takes a few days to get results. However, rapid strep tests sometimes give false-negative results (saying you don’t have strep when you really do).
Depending on your symptoms, your child’s healthcare provider may also order:
Healthcare providers sometimes use the Jones criteria to diagnose rheumatic fever. To make a diagnosis of rheumatic fever, your child must have two major criteria or one major and two minor criteria from the following lists. In addition, there must be laboratory evidence of a previous group A streptococcal infection.
Advertisement
Major criteria include:
Minor criteria include:
Rheumatic fever treatment first focuses on getting rid of the bacterial infection. Treatments then address inflammation inside your child’s body.
Treatment for rheumatic fever may include:
Rheumatic fever doesn’t have a cure, but treatments can manage the condition. Getting a precise diagnosis soon after symptoms show up can prevent the disease from causing permanent damage. Severe complications are rare. When they occur, they may affect your child’s heart, joints, nervous system or skin.
Rheumatic fever can come back or become a serious problem. In some cases, rheumatic fever can lead to serious or even life-threatening complications. Your child may need regular checkups to protect their health long-term.
Treating strep throat and scarlet fever early is essential. It can prevent rheumatic fever. Strep throat and scarlet fever symptoms aren’t always obvious or easy to spot. Call your child’s healthcare provider for guidance if your child has had a sore throat for more than three days or has other symptoms that concern you.
If your child has strep throat or scarlet fever, make sure you follow their provider’s instructions carefully. Your child needs to finish the full course of antibiotics, even if they feel better. Otherwise, the infection may not go away and may make your child more prone to rheumatic fever.
Practicing good hygiene can reduce your child’s chances of getting a bacterial infection. It can also stop your child from spreading an infection to someone else. Your child should always:
If your child’s been diagnosed with rheumatic fever, their provider may prescribe a long-term antibiotic (monthly injections of penicillin). This can help prevent future bouts of strep throat and prevent recurrences of rheumatic fever.
Yes. Your child can get rheumatic fever again if they get strep throat or scarlet fever again. If they’ve had rheumatic fever, their provider may recommend they take antibiotics for years or possibly throughout their life. This treatment is called antibiotic prophylaxis. It can prevent another strep infection and keep rheumatic fever from coming back.
If your child has rheumatic fever, you may want to ask their provider:
If you suspect your child may have strep throat or scarlet fever, don’t wait to call their provider. Early treatment can prevent rheumatic fever. Common signs of these bacterial infections include:
Rheumatic fever is a rare complication of untreated strep throat or scarlet fever. It most commonly affects children and teens. In severe cases, it can lead to serious health problems that affect your child’s heart, joints or other organs. If you suspect your child has strep or scarlet fever, take them in to see their provider right away. This can help prevent rheumatic fever. People with rheumatic fever often need lifelong medical care to protect their health.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Need care fast? Cleveland Clinic’s Express Care and Urgent Care locations treat everything from sprains to sinus infections — no appointment needed.
