Ambulatory blood pressure monitoring is a method to measure your blood pressure on a continuous basis for 24 hours. Your blood pressure is measured even as you sleep. The ongoing data helps your healthcare provider get a more accurate picture of your blood pressure numbers. The results can confirm a high blood pressure diagnosis and guide treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Ambulatory blood pressure monitoring is a way of measuring and managing high blood pressure. High blood pressure (hypertension) means your top number (systolic blood pressure) is at least 130 mmHg (millimeters of mercury), and/or your bottom number (diastolic blood pressure) is at least 80 mmHg.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Ambulatory blood pressure monitoring records your blood pressure (BP) readings over a 24-hour period, whether you’re awake or asleep. This happens outside your healthcare provider’s office, as you go about your daily life. You wear a cuff on your arm and a small device attached to a strap or belt.
You may be more familiar with having your BP checked in a healthcare provider’s office during an appointment. In this case, your provider uses a device called a sphygmomanometer to measure and record one or two readings during your visit.
Ambulatory blood pressure monitoring takes dozens of readings over a continuous period. In most cases, the device records readings every 15 to 30 minutes during the day and every 60 minutes at night. The device also measures your heart rate (how fast your heart is beating). Your provider uses this data to calculate your average BP over the 24-hour period. They also calculate changes in BP and heart rate, BP distribution pattern and other statistics.
Healthcare providers use this method for many reasons, including to:
Advertisement
Ambulatory blood pressure monitoring can detect abnormal changes in BP that might otherwise go unnoticed. It’s a useful way to detect different blood pressure patterns, as listed below.
Some people who have normal blood pressure at home have elevated blood pressure in a healthcare setting. This is known as white coat hypertension, or white coat syndrome. It can lead to a hypertension diagnosis when your blood pressure is actually normal. White coat hypertension occurs in 10% to 30% of people with elevated BP readings in healthcare settings.
Current guidelines don’t recommend treatment when ambulatory monitoring shows normal readings outside your provider’s office. However, research continues to explore this topic. White coat hypertension may still indicate a blood pressure problem. So, you and your provider should keep an eye on it.
This refers to BP readings that are elevated whether you’re in your provider’s office or at home. Researchers have linked this condition to an increased risk of heart and kidney damage, as well as stroke.
This occurs when your BP reading is normal at your provider’s office, but elevated when you’re at home. It may affect up to 30% of adults who have normal BP readings at their provider’s office. You may face a higher risk of developing masked hypertension if you have kidney disease, diabetes or obstructive sleep apnea.
This means your BP goes up when you sleep. Nocturnal hypertension affects at least 2 in 10 white people, and about 4 in 10 Black people. It’s more common among people who have diabetes or kidney disease. Research continues to explore how nocturnal high BP relates to cardiovascular disease.
Ambulatory blood pressure monitoring can help a wide range of people. Your healthcare provider may recommend ambulatory blood pressure monitoring if you:
Yes. Ambulatory blood pressure monitoring is an accurate and effective way to measure your blood pressure. It gives your healthcare provider better data compared with only measuring your BP at your medical appointments.
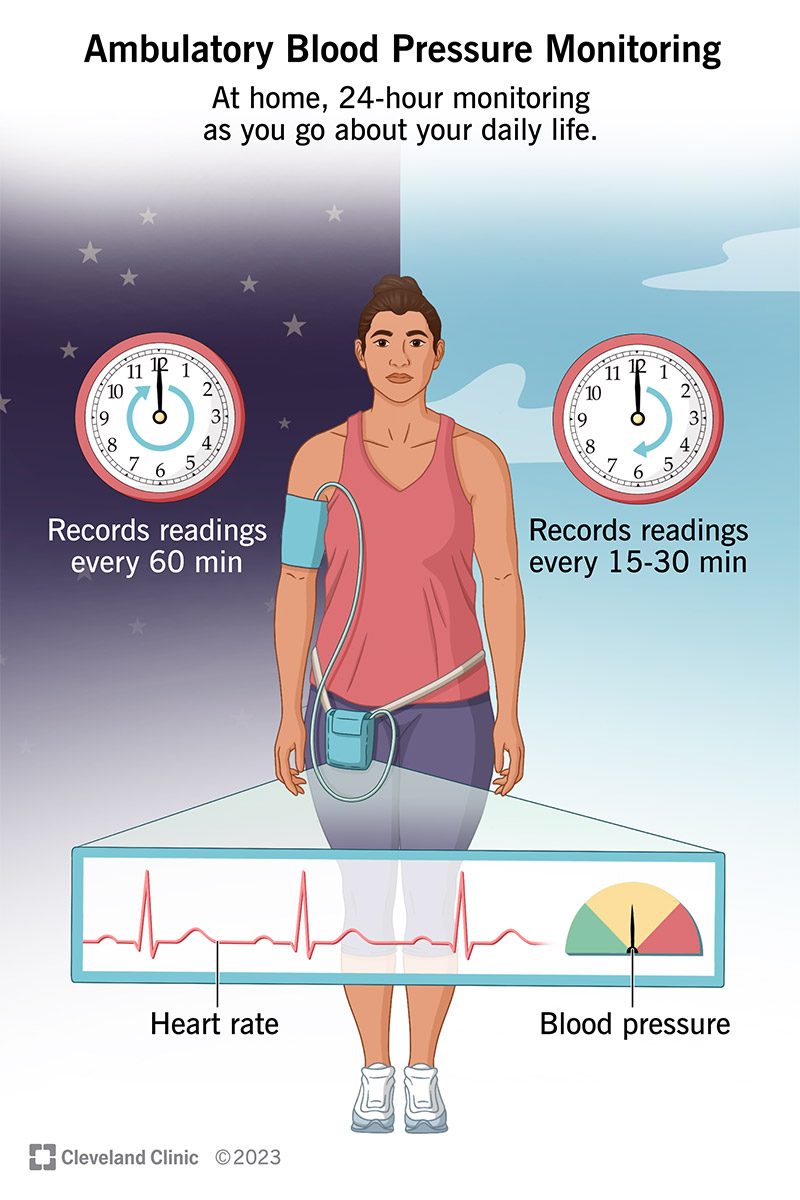
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16330-ambulatory-blood-pressure-monitoring.ashx)
Ambulatory blood pressure monitoring provides frequent readings of your blood pressure and heart rate over a 24-hour period.
Your healthcare provider will tell you how to prepare. Some general tips include:
Advertisement
Preparation also involves knowing in advance what you need to avoid. During your 24-hour period, you shouldn’t:
Ambulatory blood pressure monitoring happens outside of your healthcare provider’s office. But to get things started, you meet with your provider for an appointment. This is when you receive your equipment and instructions for the 24-hour period.
Here’s what happens at your appointment:
Advertisement
Here’s what happens once you’re home:
You may have trouble sleeping, and that’s understandable. You’re not used to having a cuff on your arm when you sleep. But try your best to relax. Do whatever you can to make the rest of your sleep environment comfortable. You may want to:
Advertisement
Your provider will tell you how you may adjust your equipment while you sleep. For example, you may be able to remove the strap from your body and place it next to your pillow. Only do this if your provider says it’s OK. You shouldn’t remove the arm cuff until the end of your monitoring period.
Talk to your provider about what you can do to get the best quality sleep.
Ambulatory blood pressure monitoring is an incredibly useful clinical tool that can help you receive the most appropriate care. Among its many benefits, this form of BP monitoring can:
This method of BP monitoring, though noninvasive, may still be uncomfortable for some people. Disadvantages include:
Your healthcare provider will transfer the data from the device to a computer, which analyzes your BP readings. Your provider will talk to you about your results and what they mean for you.
Some results your provider may discuss with you include:
These are the normal readings for ambulatory blood pressure monitoring:
Your provider will tell you when you can expect to see your results. They’ll also discuss the results with you and discuss any next steps, like medication changes.
As you complete your 24-hour monitoring, call your healthcare provider if you:
No matter how many times you tell yourself to calm down, you might still feel anxious when your provider puts a blood pressure cuff on your arm. That’s a common reaction, and it can be hard to actually relax. If that’s the case, ambulatory blood pressure monitoring can help. The device checks your BP as you go about your normal routine. It can show whether or not raised BP numbers at your provider’s office reflect what’s usually happening in your body.
Besides diagnosing white coat syndrome, this method can also help your provider diagnose and treat a range of other BP problems. Talk to your provider about how ambulatory blood pressure monitoring can help you, and what you can learn from the results.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart needs some help, the cardiology experts at Cleveland Clinic are here for you. We diagnose and treat the full spectrum of cardiovascular diseases.
