Concussions are common injuries, especially among young athletes. Most people recover without long-term effects, but it’s important not to rush your recovery. Don’t resume physical or other activities before your healthcare provider says it’s safe.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_9y29zfnb/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Let's Talk Concussion.
A concussion is a head injury that happens when your brain moves or twists inside your skull. Concussions are a type of traumatic brain injury. They’re some of the most common (and most commonly misunderstood) injuries that people experience.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Almost everyone’s heard of someone “getting their bell rung” or “seeing stars” after a hit. Those phrases might make it seem like concussions aren’t a big deal. And it’s true that concussions aren’t usually life-threatening. But the effects can be serious and last for days, weeks or even longer.
One concussion usually doesn’t cause permanent brain damage. But experiencing multiple concussions over a lifetime can change your brain’s structure or how it works, which can lead to severe complications and increase your risk of developing serious health conditions.
Concussions are very common injuries. Experts estimate that between 1 and 3 million people visit the emergency room with a concussion in the U.S. each year.
They’re especially common in young athletes. In fact, concussions account for more than half of ER visits for kids ages 5 to 18 every year in the U.S.
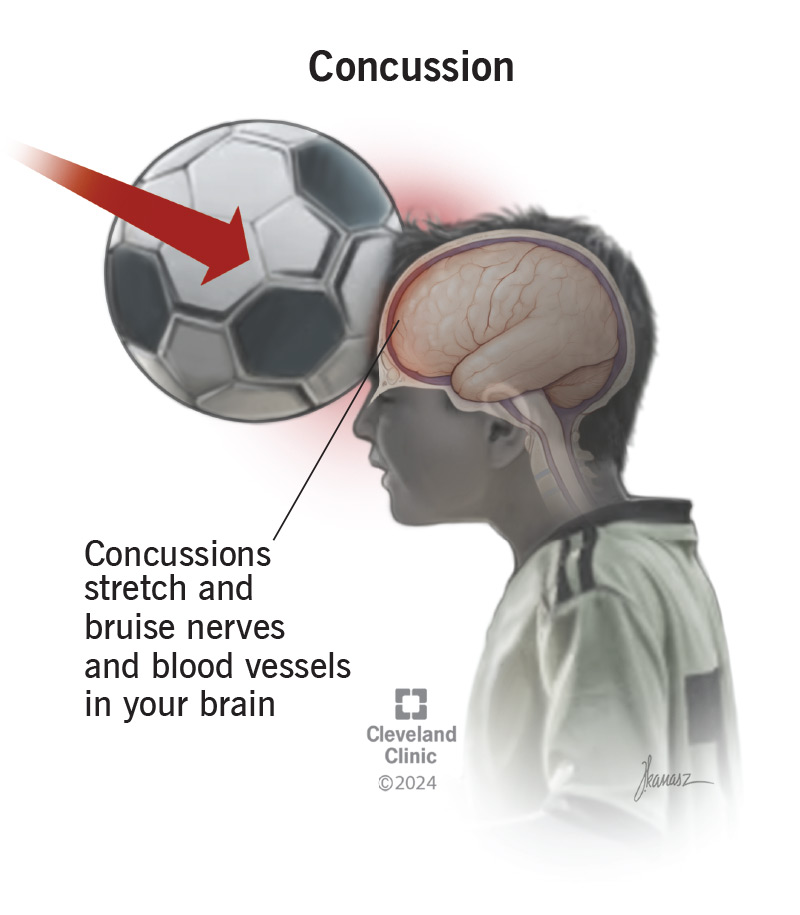
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/concussion)
Concussions stretch and injure nerves and blood vessels in your brain. They cause chemical changes that temporarily make your brain stop working like it should. Your brain will automatically redirect all its energy to healing itself after an injury. It will send signals to your body to get you to slow down and avoid activities. That’s where concussion symptoms come from. They’re your brain’s way of telling you to take it easy while it heals.
Advertisement
Concussion symptoms can affect your:
Concussion symptoms may start right away. But some people don’t experience symptoms for hours, or even days.
Physical concussion symptoms are usually the most obvious and can include:
Your cognitive function is how well your brain works and controls the rest of your body. A concussion can interfere with your brain’s normal function and cause:
Your brain controls your body’s natural sleep cycles (your circadian rhythm). It tells your body when to feel sleepy and when to wake up. A concussion can disrupt those normal rhythms, including making you:
A concussion is a physical injury that can affect your mental and emotional health. Emotional concussion symptoms can include:
Babies and kids who aren’t old enough to talk or communicate can still experience concussions. But it can be hard to know what they’re experiencing because they can’t tell you what happened or how they feel. In addition to any of the symptoms above, your child may show other signs of a concussion, including:
Everyone experiences concussion symptoms differently. But almost everyone has a headache after a concussion. It might be hard to explain, but in addition to any physical symptoms you notice, you’ll probably feel like something is “off.” You may feel dazed, stunned or like you’re in a fog. It might feel like thinking or concentrating takes effort in ways they usually don’t. Visit a healthcare provider if you hit your head and notice that you don’t quite feel like yourself.
Advertisement
Concussions happen when something jolts or shakes your body. If the force is strong enough, it can make your brain move back and forth or side to side and damage it.
Your brain tissue is soft and squishy. It’s surrounded by cerebrospinal fluid, which acts like a liquid cushion between it and your skull. Picture a glass bowl of gelatin. If you smack the bowl hard enough, the energy passes through the glass into the gelatin and makes it jiggle.
That energy transfer is what happens when you get a concussion. A strong force hits your head, neck or body, moves through your skull into your brain and makes your brain shake or wiggle. This force can twist and damage the tiny nerves and blood vessels in your brain.
The most common causes of concussions include:
Anyone can experience a concussion. People who have an increased concussion risk include:
Advertisement
Teens experience more concussions than any other age group. Researchers think this is because their brains and bodies are still developing, and they don’t always have full control of their coordination.
Only a healthcare provider can diagnose a concussion. It’s important to visit a provider if you hit your head, experience an injury or think you have any concussion symptoms.
Your provider will diagnose a concussion with a physical exam, a neurological exam or a specific concussion test. They’ll ask about any symptoms you’re experiencing and when they first started. Tell your provider if you know the exact moment or injury that caused your symptoms, and how long it took symptoms to develop after the injury or hit to the head.
During your exam, your provider will check your:
Your provider may give you tests or puzzles to evaluate your:
These tests may be written, verbal (spoken out loud) or technology-based (like on a computer or tablet).
Tell your provider if any part of the exam feels unusually hard or makes the symptoms worse. You know your mind and body better than anyone, and you can help point out if your balance is worse than usual or if it’s taking you much longer than normal to complete a puzzle.
Advertisement
Imaging tests can’t diagnose a concussion, but your provider may recommend a CT scan (computed tomography scan) or MRI (magnetic resonance imaging) to look for serious complications like bleeding in or around your brain.
Rest is the most important part of treating a concussion, especially at first. Your brain and body need time to heal. You’ll need to take a break from all intense physical exercise — especially the sport or activity that caused the concussion.
Most people need at least a few days of little or no activity. But everyone’s needs are different, and everyone’s brains heal at different rates. Your provider will recommend how long to rest, and when it’s safe to slowly resume physical or mentally challenging activities.
Learn to recognize the triggers that bring on concussion symptoms. Start adding activities back to your daily routine slowly, in small amounts. When symptoms occur, back off and rest. Once you feel better, you can attempt the activity again. But be prepared to take another break if the symptoms return.
Pace yourself. Don’t push your body to do things that make you feel worse — it’s OK to take the time you need to rest and heal. Limit any activities that worsen your symptoms.
Any activity that takes a lot of concentration may trigger concussion symptoms. Especially for the first day or two after a concussion, you may need to avoid:
Your provider may recommend that you take time off work, or that your child stay home for school for a few days. They’ll tell you when it’s okay to gradually ease back into working or doing schoolwork based on how long it takes the symptoms to get better.
You may also need to avoid:
Yes, sleep is an extremely important part of recovering from a concussion.
It’s a common myth that you shouldn’t let someone with a concussion fall (or stay) asleep. Another common myth is that you have to wake someone with a concussion up every few hours or at a set interval to make sure they’re OK. Both of these are outdated assumptions and aren’t true or necessary.
Sleep as often and as long as you naturally feel the need to. If you’re caring for someone with a concussion, it’s OK to check on them every few hours to make sure they’re breathing normally and not tossing and turning restlessly. But you don’t need to forcibly wake them up.
You shouldn’t take any over-the-counter (OTC) pain medications if you think you have a concussion before you see a healthcare provider. Many of these medications thin your blood, which can be extremely dangerous if you have a brain bleed.
Your provider will tell you which medications are safe to take while you recover. You may have to avoid NSAIDs like naproxen or ibuprofen, but it may be safe to take acetaminophen.
Tell your provider which prescription medications you take and any over-the-counter supplements you use. They’ll tell you if you need to avoid or stop any of them while you recover.
Concussions usually last a few weeks, up to a month. But everyone’s bodies respond to concussions differently. Some people naturally heal faster, and others take more time. This usually doesn’t mean you’re more or less likely to experience complications.
How long it takes your brain to heal will depend on a few factors, including:
Talk to your provider before resuming your usual daily routine. Don’t return to exercise, training or playing sports until your provider says it’s safe. Giving your body the time it needs to heal doesn’t mean you’re weak. And rushing your recovery to get back to practice, games or training doesn’t mean you’re extra tough. Your brain will heal at its own pace, and the only thing you can do to help it along is rest.
Concussions (especially repeated concussions) can cause some serious complications.
Post-concussion syndrome (PCS) happens when recovering from a concussion takes an unusually long time. You might experience symptoms for much longer than usual (four months, a year or even longer) after the original injury.
Other complications are rare, but can include:
People who’ve experienced one concussion have an increased risk for another, more serious concussion if they return to physical activities or sports too soon. Providers call this second-impact syndrome (SIS). SIS increases your risk of severe complications like brain swelling and bleeding. SIS can be fatal.
Experiencing multiple concussions and other head injuries increases your risk of chronic traumatic encephalopathy (CTE). CTE affects how areas of your brain function, communicate and work with each other.
Repeated concussions may also increase your risk of other health conditions, including:
Concussions are injuries that happen suddenly. Because you can’t plan for them, you may not always be able to prevent one. These general safety tips may reduce your risk:
Go to the emergency room if you experience a head injury and have any concussion symptoms, even if they don’t start for hours or days.
Go to the ER or call 911 (or your local emergency services number) right away if you experience any of the following symptoms:
These symptoms can all be signs of a severe complication like a brain bleed.
You may want to ask your provider:
Your brain and body are totally unique to you. And that means how you experience and recover from a concussion will be, too. Recovery doesn’t always happen in a way that we’d expect — it might take more or less time at certain stages. Be honest with yourself and your healthcare providers as you recover.
It’s scary to think about having a brain injury — especially if your child gets a concussion. But most people can recover with no long-term effects or complications. Don’t rush your recovery — the best thing for your brain is to give it all the time it naturally needs to heal itself.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
From sudden injuries to chronic conditions, Cleveland Clinic’s orthopaedic providers can guide you through testing, treatment and beyond.
