Sleep disorders are conditions that affect the quality, amount and timing of sleep you’re able to get at night. Common sleep disorders include insomnia, restless legs syndrome, narcolepsy and sleep apnea. Sleep disorders can affect your mental health and physical health. Treatment is available to help you get the rest you need.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Sleep disorders are conditions that affect your ability to get the rest your body needs and maintain wakefulness. There are over 80 sleep disorders that impact:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Everyone can experience problems with sleep from time to time. But you might have a sleep disorder if:
The categories of sleep disorders have changed many times over the years. Most recently, the International Classification of Sleep Disorders (ICSD) categorized sleep disorders based on the symptoms, how they affect a person (pathophysiology) and the body system it affects. The brand-new revision to the third edition, ICSD-3R includes the following categories:
Advertisement
The ICSD updates regularly to include the most recent information about sleep disorders and the types that fall under these categories.
There are over 80 different types of sleep disorders. The most common include:
Everyone needs sleep. It’s an essential part of what makes our bodies function. The amount of sleep you need might be more or less than others, but experts recommend adults get seven to nine hours of sleep per night. Optimal sleep time varies by age; for example, children and teenagers may need more sleep than adults.
More than 50 million people in the United States have a sleep disorder. In addition, more than 100 million Americans of all ages report that they don’t get an adequate amount of sleep.
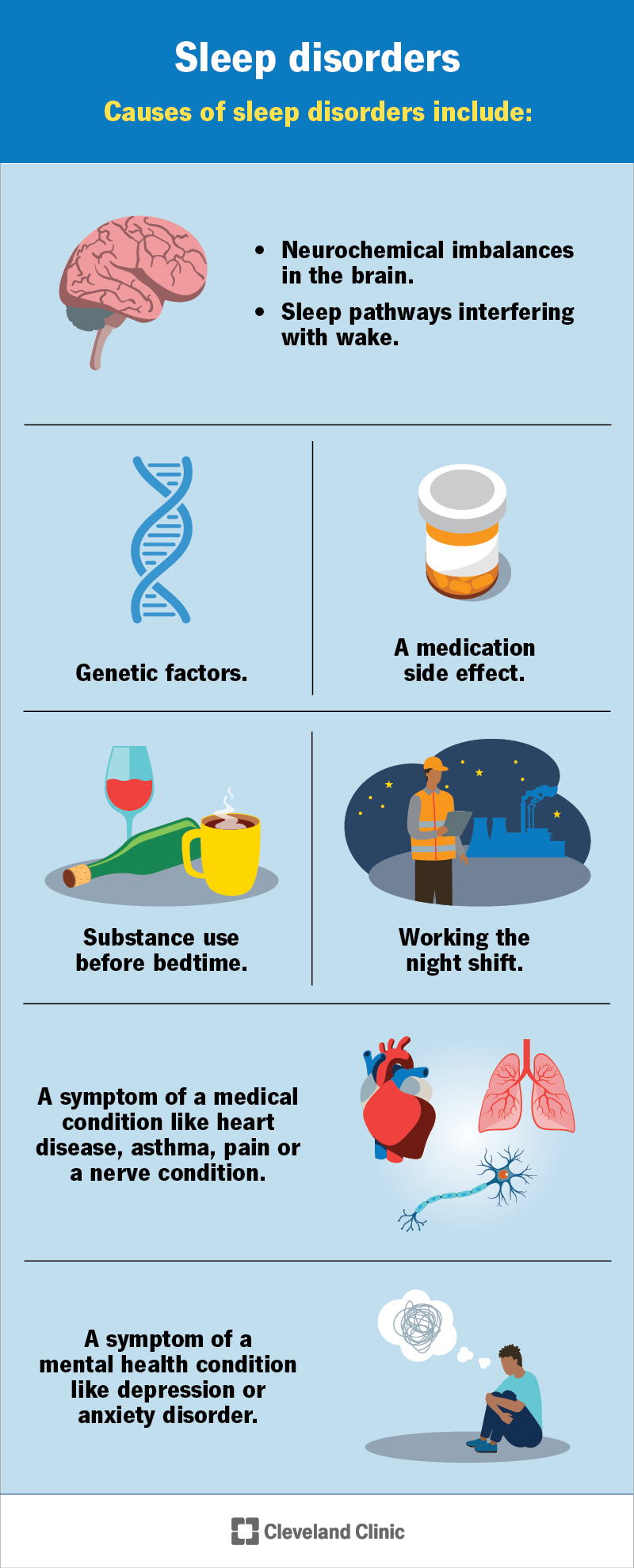
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/11429-sleep-disorders)
Symptoms of common sleep disorders vary based on the type, but could include:
During the daytime, you may experience additional signs and symptoms caused by a lack of adequate sleep, including:
If you feel like you’re not able to get a good night’s rest or have symptoms that interfere with your daytime activities, talk to a healthcare provider.
Advertisement
A disruption to your body’s cycle of sleep and daytime wakefulness causes sleep disorders. Specific things may cause this to happen, and it varies based on the type of sleep disorder you have. They may include:
You may be more at risk of sleep disorders if you:
Research suggests that females are more likely to experience sleep disorders than males.
In addition, about half of all adults over the age of 65 have a type of sleep disorder.
If you don’t get the proper amount or quality of sleep that your body needs, it can affect you beyond feeling tired during the daytime. A lack of adequate sleep can lead to:
Advertisement
Sleep loss can also contribute to the development of health conditions like:
While rare, some sleep disorders can be life-threatening.
A healthcare provider will diagnose a sleep disorder after a physical exam to review your symptoms and testing. Tests can help your healthcare provider learn more about what’s causing your symptoms like blood tests or imaging tests.
They may ask you to keep a sleep diary. A sleep diary is a record of your sleeping habits. You’ll make note of when you go to bed, when you fall asleep and when you wake up each day. You should also make note of any naps you take during the daytime and how you feel before and after sleeping.
It helps to keep a pen and piece of paper near your bed so you don’t forget to write these items down. It can be difficult to know what time you fall asleep exactly, so you should estimate what that time is. You might choose to wear a smartwatch or a device (actigraph) that records your cycles of rest and activity. This can confirm what time you fell asleep and woke up.
Your primary care provider may recommend you visit a sleep specialist who’ll perform a sleep study (polysomnogram). A sleep study is a sleep disorder test that electronically transmits and records specific body and brain activities while you sleep. A healthcare provider will analyze the sleep study data to determine whether or not you have a sleep disorder.
Advertisement
To learn more about concerns you have about your sleep patterns, a healthcare provider may ask the following questions during an exam:
Your healthcare provider may refer you to a sleep specialist if they suspect you have a sleep disorder. A sleep specialist is a highly trained healthcare provider who specializes in how sleep affects your body.
There are several types of treatment options available for various sleep disorders, which could include:
Your healthcare provider will recommend treatments based on your situation. They’ll also discuss any side effects to look out for before you begin treatment.
Your healthcare provider may recommend some of the following medications and supplements to treat common sleep disorders:
A healthcare provider may recommend you make changes to your sleep hygiene so you can sleep better. Sleep hygiene includes making changes to your sleeping routine to create an optimal sleeping environment. You can get better sleep by:
Sleep disorders can affect your overall health. You may not have the energy to do the things you want to do or even complete your daily routine. You may miss out on special moments or events because your sleep disorder prevents you from being fully present. In addition, you may put yourself and others at risk, especially if you drive or operate heavy machinery and aren’t getting the rest you need to stay safe.
If you’re struggling to get quality sleep where you wake up feeling refreshed, talk to a healthcare provider. Treatment is available to manage many sleep disorders and get you back to wellness.
There isn’t a specific time limit as to when a sleep disorder will stop affecting you. You may be able to find a treatment that makes you feel better within weeks to months. Others may need to manage the condition throughout their lifetime. Talk to your healthcare provider about your specific outlook.
You can’t prevent all types of sleep disorders, but you can reduce your risk by practicing good sleeping habits (sleep hygiene).
You should avoid the following three to four hours before bedtime if you want to improve your sleep:
Talk to a healthcare provider if you’re having trouble with sleep and wakefulness. This could be falling asleep, staying asleep or awake, getting restful sleep or unexplained daytime sleepiness or tiredness.
Sleep disorders affect your quality of life. They can disrupt your thinking, school or work performance, mental health and physical health. Common sleep disorders prevent you from getting the restful, deep sleep you need to function at your best. If you’re struggling with your sleep, don’t hesitate to see a healthcare provider. Your health and, therefore, quality of life depends on good sleep. Practice good sleep hygiene and follow your healthcare provider’s instructions to feel better sooner.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When sleep disruptions, snoring, abnormal behaviors during sleep or being tired all day gets to be too much, sleep testing at Cleveland Clinic can provide answers.
