Dissociative identity disorder (DID) is a mental health condition where you have two or more separate personalities that control your behavior at different times. When personalities switch, you’ll have gaps in your memory. The identities are usually caused by living through trauma. Psychotherapy can help you manage your symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Dissociative identity disorder (DID), formerly known as multiple personality disorder and split personality disorder, is a mental health condition where you have two or more separate identities.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Dissociate” means to separate or disconnect. People with dissociative identity disorder may experience several different personalities, usually referred to as alters. Each identity may have different behaviors, memories, thought patterns or expressions. The identities might have different ethnicities and ways of interacting with their environments.
These personalities may control your behavior at different times. Memories may not transfer from one identity to another, which can cause amnesia (gaps in memory). The presence of amnesia is often an important symptom that raises concern for the diagnosis.
DID interferes with your ability to function in your day to day. It can impact your relationships with others and performance at school or work.
DID is one of several dissociative disorders. These disorders affect your ability to connect with reality.
There are two types (or forms) of DID:
Advertisement
It’s important to note that possession is a common belief of different cultures and religions around the world, but these voluntary spiritual practices aren’t associated with DID.
DID isn’t common. One small U.S. study found that DID affects an estimated 1.5% of people.
Current estimates on how common this condition is may vary based on new diagnostic criteria introduced in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5).
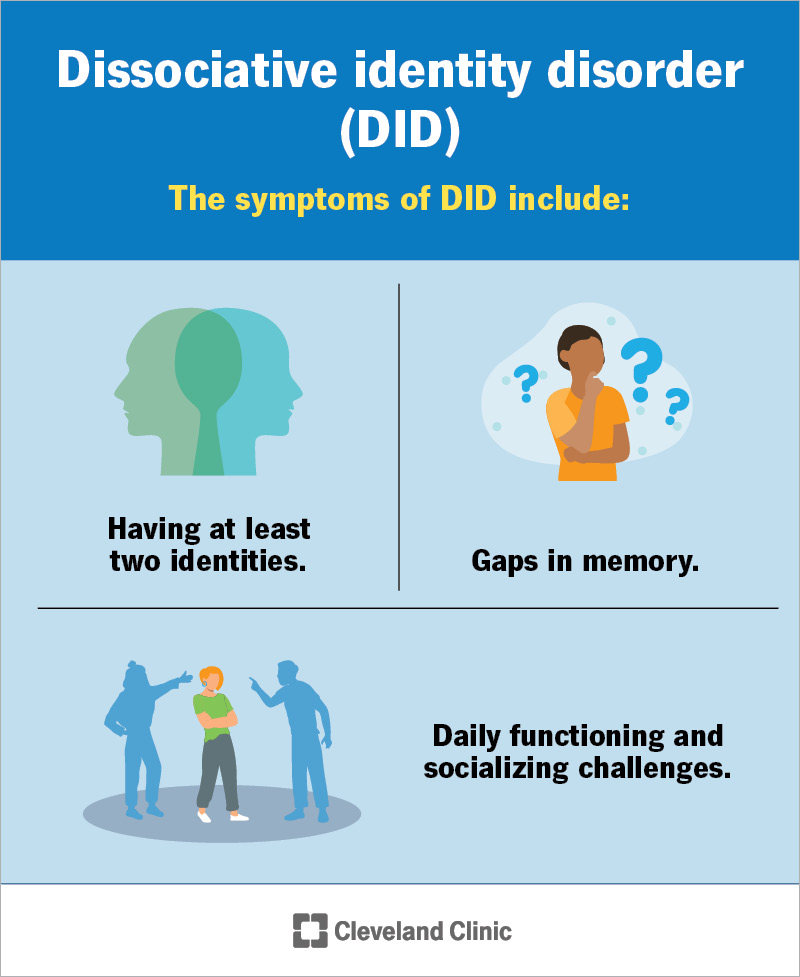
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9792-dissociative-identity-disorder-multiple-personality-disorder)
The symptoms of DID include:
Other mental health symptoms that can (but not always) be found along with DID include:
If you have DID, you might feel or experience the following:
It doesn’t feel like you’re “you” with DID. This can look and feel different for each person who experiences it. If something doesn’t feel right or your experiences and memories aren’t lining up, reach out to a healthcare provider for an evaluation.
Yes, it’s possible that someone can have DID without knowing. While some people are aware of their identities, many people don’t know when a new identity takes over. When a new identity steps in, you may not remember some events because another personality experienced them. This causes gaps in memory, called amnesia.
DID causes may include:
These events typically happen during childhood. DID is a way for you to distance or detach yourself from the trauma.
DID symptoms may trigger (happen suddenly) after:
You may be more at risk of developing DID if you experienced:
Advertisement
You’re at an increased risk of suicide with DID. More than 70% of people diagnosed with DID attempt suicide or practice self-injury behaviors.
If you’re thinking about hurting yourself, call or text 988, the Suicide & Crisis Lifeline (U.S.). You don’t have to be in a crisis to dial 988. Someone is available to talk, no matter your situation, so you can feel better in your time of need.
A healthcare provider, usually a psychologist and/or psychiatrist, will diagnose DID after taking a detailed medical history and learning more about you and your symptoms. Your provider may gather more information from people who know you best or spend the most time with you. Usually, someone close to you will be the first to notice a change in your personality and raise concerns.
There isn’t a single test that can diagnose DID. A provider will likely run a physical exam and neurological exam, among other tests, to rule out any conditions that could cause symptoms. They’ll review your symptoms and compare them to the criteria presented in the American Psychiatric Association’s Diagnostic and Statistical Manual, 5th edition.
In addition, your provider may use different questionnaires or scales to evaluate dissociative behavior. These include:
Advertisement
Your provider will also ask you questions to learn more about your risk of suicide, as it’s common among people who experience DID.
Symptoms of DID often show up in childhood, between the ages of 5 and 10. But it’s common for parents, other family members, guardians, teachers or healthcare providers to miss or mistake the early signs. They may confuse DID with other behavioral or learning challenges, such as attention-deficit/hyperactivity disorder (ADHD). For this reason, DID usually isn’t diagnosed until adulthood.
Due to the rarity of DID and the large variation in symptoms, it may take even experienced healthcare providers time to make an accurate diagnosis.
Treatment for DID includes:
The first step of treatment is always to make sure you’re safe. A healthcare provider with specialized training in mental health disorders can guide you toward the right treatment. Treatment focuses on meeting your specific needs.
Advertisement
Therapy for DID focuses on:
You may benefit from individual, group or family therapy.
Participating in therapy is challenging. You’ll need to work through events that bring strong emotions. These can make you feel anxious, helpless, scared and alone. But you’re not alone. Your therapist and loved ones are willing to help and support you as you navigate treatment for DID.
Some healthcare providers recommend hypnotherapy in combination with psychotherapy. Hypnotherapy is a form of guided meditation. It may help you recover suppressed memories.
There isn’t a cure for DID. But your symptoms can get better. You’ll need to manage the condition for your entire life. This can feel overwhelming, but your provider will help you find the right treatment or combination of treatments so symptoms don’t take over.
There’s no way to prevent DID. However, identifying signs as early as possible and seeking treatment can help you manage symptoms. Parents, caregivers and teachers should watch for signs in young children. Treatment soon after episodes of abuse or trauma may prevent DID from progressing.
Treatment can also help identify triggers that cause personality or identity changes. Managing stress and avoiding non-prescribed drugs and overconsumption of alcohol may help reduce the frequency of different alters controlling your behavior.
Always follow your provider’s treatment plan. This could include taking medications as directed and continuing treatment, even if you feel better. If things are difficult or you notice things get worse instead of better, let your provider know immediately. They can work with you to adjust your treatment plan throughout your life.
A strong support system can make living with DID more manageable, too. Make sure you have healthcare providers, family members and friends who know about and understand your condition. Communicate openly and honestly with the people in your support system. Don’t be afraid to ask for help when you need it.
Having a loved one with DID can be confusing and overwhelming. You may not know how to respond to their different alters or behaviors. You can help by:
It’s easy to minimize the impact that your symptoms have on your daily routine. If you suspect something isn’t right about your sense of self, your memory or how you’re able to function, contact a healthcare provider.
If you or someone you know has DID and exhibits any of the following, seek medical attention right away:
In the U.S., you can call or text the Suicide and Crisis Lifeline by dialing 988. This hotline connects you to a network of local crisis centers that provide free and confidential emotional support. The centers support people in suicidal crisis or emotional distress 24 hours a day, seven days a week.
If you or a loved one are in immediate danger, call 911 or your local emergency services number.
Dissociative identity disorder (DID) is a mental health condition where you have two or more separate identities. It can be a way for you to escape from negative experiences you’ve lived through. To protect yourself and move forward, you might have placed your trauma in a box and tucked it away in the back of your brain.
While DID provides an escape from reality, it can take you away from your loved ones and your true self. A mental health professional can help you work through these difficult experiences to open that box carefully when you’re ready. Together, you’ll sort through the contents to better organize the challenges you experienced. While you’re going through therapy, it helps to build a strong support system of people you can rely on when you don’t feel like yourself. Remember, you’re not alone as you manage DID.
Over time and with the right treatment, you can function better and feel more in control of your true self.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Your mental well-being is just as important as your physical well-being. Cleveland Clinic’s mental health experts can help you live life to the fullest.
