A vasectomy is a type of surgery that provides a permanent birth control. A surgeon separates your vas deferens so sperm can’t enter your semen. It’s a safe, effective and quick procedure that typically takes about 30 minutes to perform. Most people make a full recovery within 10 days.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
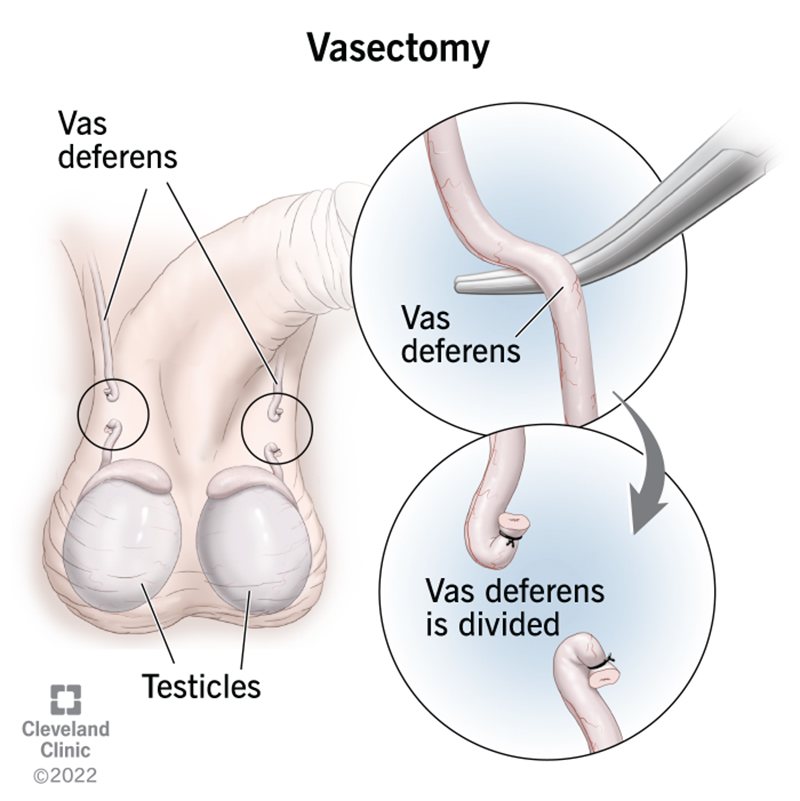
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4423-vasectomy)
A vasectomy (va-SEK-tuh-mee) is a surgical procedure that stops sperm from mixing with your semen and leaving your body. It’s a permanent type of birth control (contraception). The procedure closes off the ends of your vas deferens. The vas deferens is a tube that carries sperm to your urethra.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A vasectomy is a safe, common and effective procedure for preventing pregnancy. But it doesn’t protect you from sexually transmitted infections (STIs).
After a vasectomy, your testicles continue making sperm. When the sperm cells die, they disintegrate, and your body absorbs them. This is the same way your body handles other types of cells that die and are replaced every day.
A vasectomy won’t affect your:
The only way to absolutely avoid getting pregnant is to avoid sexual intercourse (practice abstinence). But vasectomies are very effective at preventing pregnancies.
The failure rate of vasectomy is very low. In rare cases, after a vasectomy, it’s possible for sperm to cross the separated ends of the vas deferens. A 2016 study shows there’s a higher chance of having sperm in your semen three to six months after a vasectomy — 0.3% to 9%. But after that period, the failure rate range drops below 1%. This rate is lower than any other form of birth control. For example, even when used correctly, a 2017 study states that condoms fail to prevent pregnancy around 2% of the time.
Vasectomies are very common. In the U.S., more than 500,000 people get a vasectomy every year.
Advertisement
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_5jjoe3zd/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn what to expect before, during and after a vasectomy.
Before you have a vasectomy, certain things should happen.
Before a vasectomy, you should talk with your partner and a healthcare provider about the procedure. You should be sure that you don’t want to have any biological children. You should consider a vasectomy a permanent form of birth control. Although it’s possible to undo a vasectomy, it isn’t always successful. It can also be expensive.
During your consultation, the provider will also ask you questions, including:
The provider will explain the vasectomy procedure to you and ask for your consent. This means you:
Before you sign any forms, make sure you don’t have any questions and are comfortable with your decision. It’s important to resolve any concerns before the procedure. Remember: A vasectomy is an elective procedure. You don’t have to do it unless you’re sure it’s the right choice for you.
The night before or the morning of your vasectomy, shave away the hair from your entire scrotum. Remove the hair all the way to the top of your penis, including any pubic hair that falls down to your scrotum. Don’t use an electric razor on your scrotum. A single-blade disposable razor is the best choice.
To reduce your risk of infection, thoroughly wash your scrotum and groin with antibacterial soap and warm water the day before and the morning of your surgery. Be sure to completely dry the area, too.
Other ways in which you can prepare for a vasectomy include:
Advertisement
A vasectomy team generally consists of a urologist and nurses. A urologist is a surgeon who specializes in the urinary system and reproductive system. Nurses assist the urologist during the procedure.
There are two types of vasectomies:
Healthcare providers perform both types in an office or outpatient surgery center. They both use local anesthesia to numb your scrotum. You may receive the local anesthesia as a shot or a spray.
Each type divides and closes off the ends of your vas deferens to prevent sperm from mixing with your semen and releasing when you ejaculate, usually during an orgasm. But during an incision vasectomy, a urologist uses a surgical knife (scalpel) to make one to two small cuts (incisions) in your scrotum. A no-scalpel vasectomy doesn’t involve incisions. A urologist uses a small instrument to create a hole in your scrotum and gently spread it open a little.
During both types of vasectomy, once the urologist creates an opening, they’ll:
Advertisement
A urologist only removes a small section of your vas deferens during a vasectomy. They don’t remove your testicles or any other part of your reproductive system.
A vasectomy is a relatively quick procedure. Urologists typically complete the procedure in about 15 minutes. But it may be even faster.
After your vasectomy is complete, a healthcare provider will cover any stitches with bandages and monitor your overall health. Once they determine you’re okay, they’ll let you go home.
A provider will conduct a semen analysis about two to three months after your vasectomy to check your semen for sperm.
As a method of birth control, a vasectomy has many advantages. The main benefit is that it’s the most effective form of birth control besides abstinence.
Like “getting your tubes tied” (tubal ligation), a vasectomy is a one-time procedure. But when compared to getting your tubes tied, a vasectomy is:
A vasectomy also relieves your partner of any birth control stresses, such as taking birth control pills every day or their side effects.
A vasectomy shouldn’t change your ability to delay orgasm. But it might increase your comfort level with sexual intercourse by reducing any stress related to pregnancy.
Advertisement
Some people are able to achieve greater control of their orgasms with Kegel exercises.
Like any type of surgery, complications can occur after a vasectomy. These may include inflammation, bleeding or infection. But they’re not common and usually aren’t serious.
Other minor risks include:
Any procedure can affect your nerves. Rarely, this may cause long-term testicular pain after the procedure (post-vasectomy pain syndrome). Post-vasectomy pain syndrome may also cause pain when you ejaculate (dysorgasmia or orgasmalgia) and psychological distress.
It’s not clear to healthcare experts if a vasectomy increases your risk of post-vasectomy pain syndrome or why it develops. It’s a complex condition that affects 1% to 2% of people after a vasectomy. But it’s treatable.
A sperm granuloma is a hard, sometimes painful lump about the size of a pea that may develop from sperm leaking from your cut vas deferens. The lump isn’t dangerous, and your body almost always absorbs it. Pain relievers and supporting your scrotum with a jock strap or compression shorts can help relieve symptoms.
Scrotal congestion is a sense of discomfort or pressure you may feel in your:
Congestion may occur two to 12 weeks after a vasectomy. But it usually resolves itself over time.
In very rare cases, it’s possible for your vas deferens to reconnect (recanalization), even years after a successful vasectomy. Your epididymis still carries sperm to the severed ends of your vas deferens. Tiny tubes may develop in white blood cell clusters at the ends (granulomatous tissue), which creates a new connection (fistula).
Most recanalizations occur during the first 12 weeks after a vasectomy (early recanalization). Scheduling a semen analysis a few months after the procedure ensures you’ve cleared all sperm from your vas deferens and that the ends of your vas deferens didn’t reconnect.
Before a vasectomy, it’s common to wonder if the procedure will affect your testosterone levels, sex drive and semen. You may even worry if your partner will be able to notice any differences.
A vasectomy won’t affect how your body produces or releases testosterone. It also won’t affect your sexual abilities — your erections and orgasms will be the same, and there won’t be any changes in the amount of semen you release or how it looks or tastes. The only difference is that your semen will no longer carry sperm (azoospermia).
Some people report that sexual intercourse with their partners is more impulsive and enjoyable because they no longer have to worry about pregnancy or interrupt intercourse to deal with contraception, like condoms.
Many studies suggest that there aren’t significant risks to your long-term health after a vasectomy. Getting a vasectomy won’t increase your odds of developing any conditions or issues, including cancer or heart disease.
Most people report a full recovery eight to nine days after a vasectomy. But you can resume many of your everyday activities within a few days (usually 48 to 72 hours) after the procedure.
It’s important to use caution when exercising after a vasectomy. Start with walking and standing for longer periods. Avoid lifting anything heavier than 10 pounds (4.5 kilograms) — about a gallon of water. Stop if you have any discomfort, pain or swelling. To make sure you completely heal, it’s a good idea to avoid strenuous exercise (for example, powerlifting, contact sports, martial arts and mountain biking) for at least a month.
Most people can go back to work or school in less than a week. But you may need to take more time off if you have a physical job that involves a lot of heavy lifting or exercise.
Your body needs time to heal after a vasectomy. You should refrain from all sexual activity, including masturbation, for at least seven days after the procedure. When you have sexual intercourse again, use another form of birth control until your semen analysis shows you no longer have any sperm in your semen.
No. After a vasectomy, sperm can remain in your vas deferens for weeks or even months. Be sure to schedule a semen analysis two to three months after the procedure to confirm that your semen no longer contains sperm. If a semen analysis shows sperm, a healthcare provider will recommend repeating the test about a month later. Until then, you must use other birth control methods to prevent pregnancy.
A semen analysis is the only way to ensure there’s no sperm in your semen. If you don’t confirm there’s no longer sperm in your semen, you run the risk of getting your partner pregnant if you have unprotected sexual intercourse.
You can help clear sperm by ejaculating frequently, starting around a week after a vasectomy. Frequent ejaculations help increase your chances of a sperm-free semen analysis.
Call a healthcare provider if you have signs of infection after a vasectomy, including:
Getting a vasectomy is a personal decision. Many choose to get a vasectomy because it’s an effective way to prevent pregnancy. Some people choose to get a vasectomy because they don’t wish to have biological children or any more children. But you may wish to get a vasectomy to protect your partner’s health if pregnancy is a health risk. It also helps prevent genetic disorders in a child.
Healthcare providers perform vasectomies under a local anesthetic, so you won’t feel much discomfort. But some people describe a “tugging” sensation or feeling of things moving around.
Once the local anesthesia wears off, most people describe the pain as moderate. You can help manage your pain by icing the area and taking recommended pain relievers.
Yes, a vasectomy reversal is an option if you decide you want another biological child.
You may also consider sperm banking before a vasectomy. Many people who decide to reverse their vasectomies choose to do so because they want biological children with a new partner. But banking your sperm allows you to freeze and store it for later use without a vasectomy reversal.
Talk about the procedure with your partner. If you’re thinking about a vasectomy reversal now, you may need more time to decide if a vasectomy is right for you.
No, you can’t have a biological child after a successful vasectomy without banking your sperm or getting a vasectomy reversal.
It depends on many factors, including:
Talk to a provider. They can refer you to a patient financial coordinator who may be able to help estimate the cost of a vasectomy reversal.
It’s a big decision to get a vasectomy, and it’s a good idea for you and your partner to give it a lot of thought. It’s possible to reverse some vasectomies. But don’t have the procedure unless you’re sure it’s what you and your partner want.
If you’re confident a vasectomy is the right choice for you, you should know that the procedure is safe, effective, less costly and more convenient than most other forms of birth control. Reach out to a healthcare provider if you have any questions or concerns.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Getting a vasectomy can be a life-changing decision. When you’re ready, Cleveland Clinic’s here to help.
