Joint hypermobility syndrome is a genetic condition that involves extreme flexibility along with pain and other symptoms. Many people have very flexible joints. But if you also have pain and other symptoms, it may be joint hypermobility syndrome. While there’s no cure, symptoms can be managed by keeping your muscles strong and taking medication.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Joint hypermobility syndrome is a connective tissue disorder. Thick bands of tissue (ligaments) hold your joints together and keep them from moving too much or too far out of range. In people with joint hypermobility syndrome, those ligaments are loose or weak. If you have joints that are more flexible than normal and it causes you pain, you may have joint hypermobility syndrome.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Joint hypermobility is very common. Hypermobility means your joints can move beyond the normal range of motion. You may also hear the term double-jointed. This means your joints are very flexible. The most commonly affected joints are your elbows, wrists, fingers and knees.
In most people, hypermobility doesn’t cause any pain or medical issues. However, for some people, hypermobility causes joint pain, joint and ligament injuries, tiredness (fatigue), bowel issues and other symptoms. Joint hypermobility syndrome is most common in children and young people. It affects females and people of Asian and Afro-Caribbean descent more often. It usually gets better with age.
Joint hypermobility syndrome can be a sign of a more serious underlying genetic condition. These conditions are called Heritable Disorders of Connective Tissue (HDCT). Rare medical conditions associated with joint hypermobility syndrome include:
Advertisement
The most common symptom of joint hypermobility syndrome is pain in your joints and muscles. Other symptoms may include:
The exact cause of joint hypermobility syndrome isn’t known. However, the disorder tends to run in families. The genes that are involved in the creation of collagen are believed to play a role. Collagen is the protein that adds flexibility and strength to your joints, ligaments and tendons. People with joint hypermobility syndrome have loose joints because they have weak ligaments. They have weak ligaments because of the defect in their collagen.
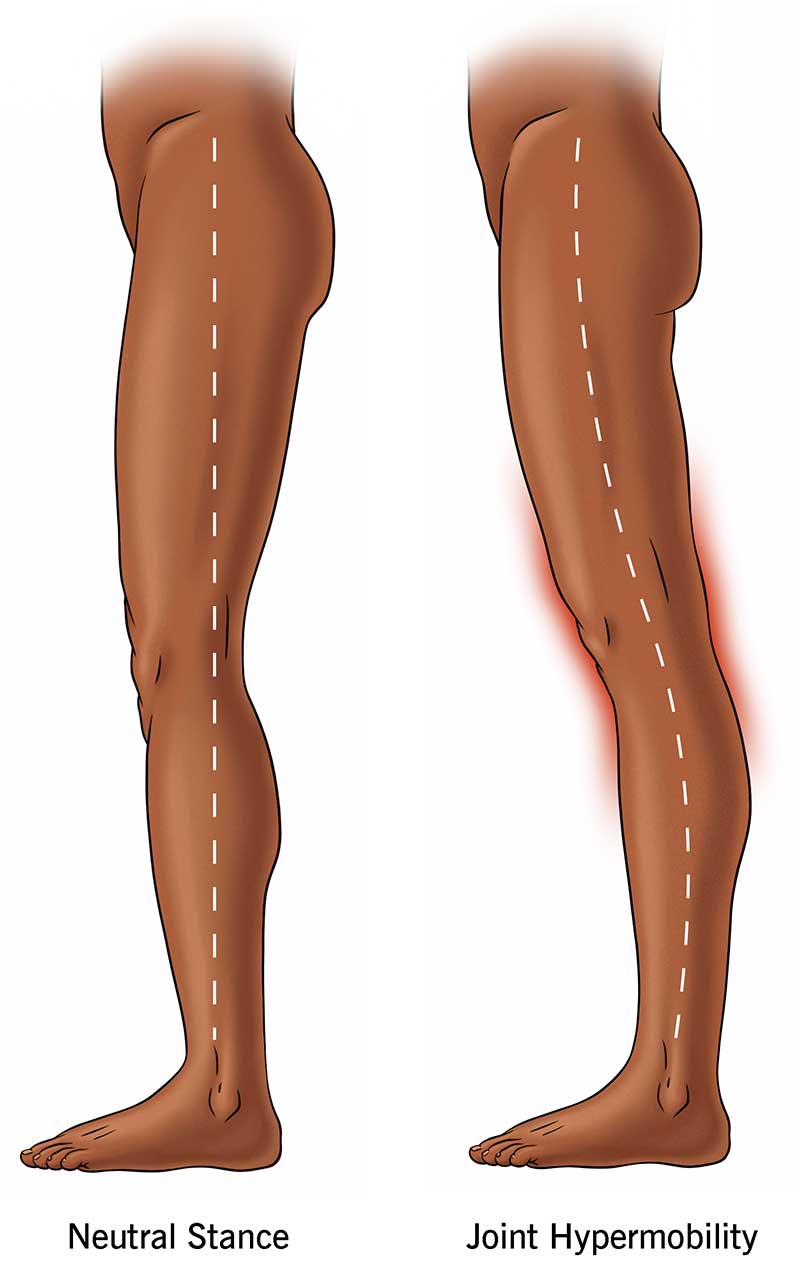
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/21763-joint-hypermobility-syndrome)
Your healthcare provider may perform a physical exam to see the range of motion in your joints. They may also order blood tests to check for possible genetic conditions.
Your healthcare provider may use a test or questionnaire to measure the flexibility of your joints. The Beighton score measures your joint flexibility on a nine-point scale. You receive one point for each of the following:
If you scored four or more points and have had pain in four or more joints for at least three months, you may have joint hypermobility syndrome.
Your healthcare provider may also ask you the five-point hypermobility questionnaire. The five questions asked are:
If you answered “yes” to two or more questions, you may have joint hypermobility syndrome.
There’s no cure presently for joint hypermobility syndrome. Treatment involves protecting your joints and managing your pain. You can protect your joints by strengthening your muscles through exercise. Other recommendations include:
Advertisement
For mild pain, your healthcare provider may recommend an over-the-counter pain reliever such as acetaminophen (Tylenol®), ibuprofen (Advil®, Motrin®) or naproxen (Aleve®). For more severe pain, your healthcare provider may prescribe stronger pain medication or provide additional resources to help manage your pain.
Joint hypermobility syndrome is most commonly found in children and adolescents. As you get older, symptoms tend to decrease. For some people, symptoms are mild. For others, pain can be severe. It’s important to work with your healthcare provider on ways to protect your joints and manage your pain.
Joint hypermobility syndrome is a genetic disorder that usually runs in families. Therefore, it can’t be prevented.
Researchers have found there may be a link between hypermobility and gastrointestinal issues such as irritable bowel syndrome (IBS). The symptoms of IBS are commonly found in joint hypermobility syndrome. Therefore, your healthcare provider may recommend an exclusion diet to test for an intolerance to certain food products. If whatever’s causing the intolerance is removed, your symptoms may resolve.
The three most common exclusion diets are:
Advertisement
If you have joint hypermobility syndrome, it’s important to maintain a healthy lifestyle and protect your joints. You can improve joint and muscle strength by:
Joint hypermobility syndrome is a connective tissue disorder. Many people are double-jointed or have very flexible joints. But when you have very flexible joints along with pain and other symptoms, it may be joint hypermobility syndrome. Joint hypermobility syndrome is diagnosed through a physical exam as well as a test or questionnaire on your flexibility. While there’s no cure, symptoms can be managed by keeping your joints strong and taking medication. Talk to your healthcare provider if you have severe symptoms. They can help you manage this condition.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.