Upper respiratory infections (URIs) are viruses and bacteria that infect your respiratory tract above your vocal cords. Symptoms can include a runny or stuffy nose, sore throat or headache. Common colds, strep throat and sinus infections are all examples of upper respiratory infections. Most URIs are caused by viruses and go away on their own.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
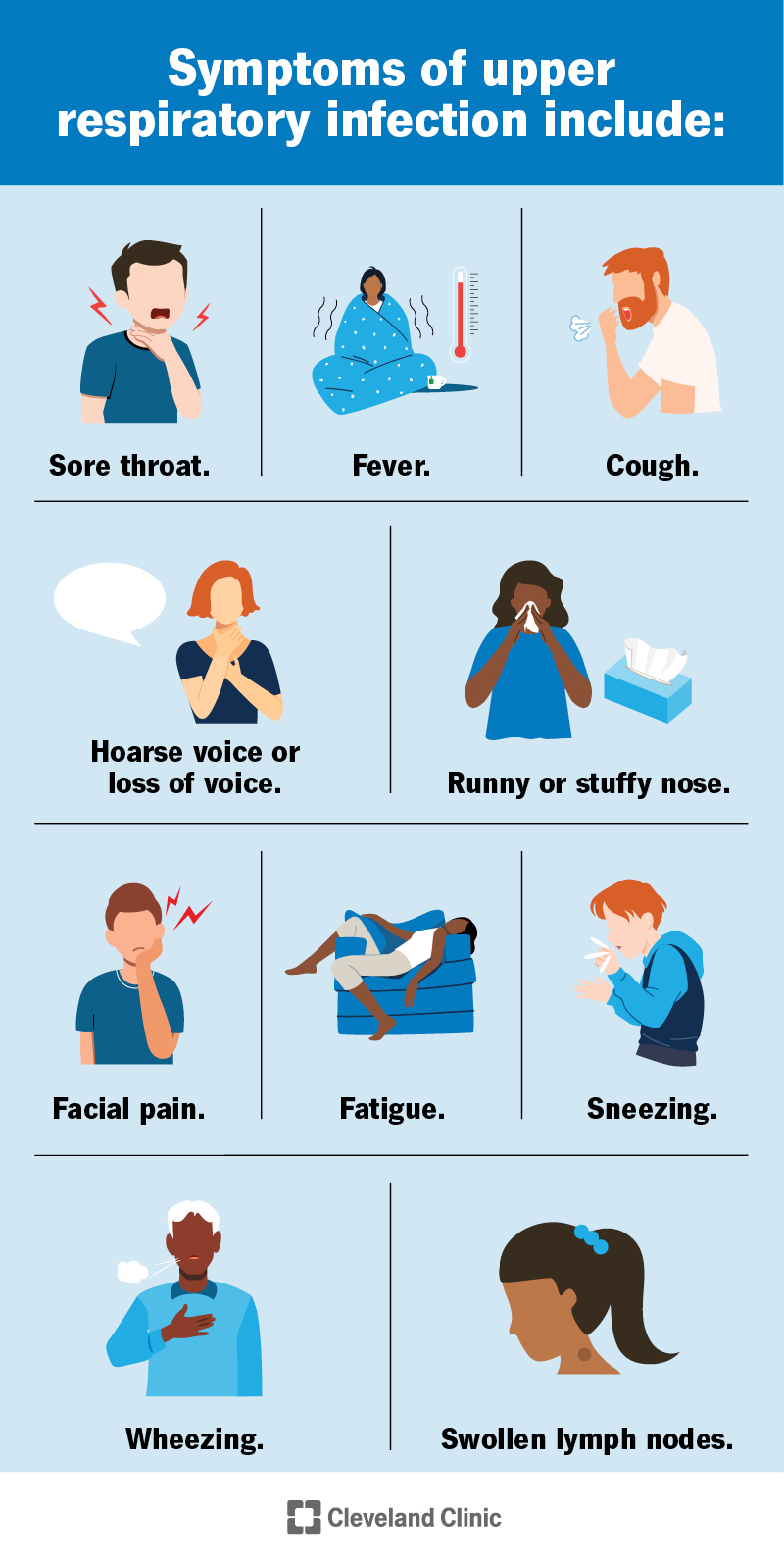
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/upper-respiratory-infection)
An upper respiratory infection (URI) is a viral or bacterial illness in the upper part of your respiratory system. This includes your nose, sinuses and throat.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A runny nose, sore throat, headache and other cold-like symptoms might come to mind when you think of an upper respiratory infection. And it’s true — common colds and other viruses are usually to blame for URIs. But some URIs, like strep throat or some cases of sinusitis, are bacterial infections. Still others, like the viruses responsible for the flu, COVID-19 and RSV, can cause both upper and lower respiratory infections.
Symptoms of upper respiratory infections depend on the cause and what part of your body is affected. Infections can lead to swelling in parts of your respiratory tract, causing conditions like pharyngitis, laryngitis and epiglottitis, which can have different symptoms.
Symptoms of upper respiratory infections can include:
Viruses cause most upper respiratory infections. But bacteria and even fungi can cause them, too. Specific causes can include:
Advertisement
Yes, the viruses and bacteria that cause upper respiratory infections are contagious (spread from person to person). They can spread through:
Fungi that cause upper respiratory infections aren’t contagious.
Upper respiratory infections like colds rarely lead to complications. But URIs can sometimes cause inflammation in your lungs, leading to pneumonia. Additionally, if bacterial or fungal infections are left untreated, they can travel to other parts of your body and cause:
You might be at higher risk for complications from a URI if you have certain health conditions or a compromised immune system, or if you’re older than 65. Newborns are also at higher risk for severe illness.
Healthcare providers usually diagnose upper respiratory infections based on your symptoms and nasal swab or throat culture. If your symptoms are mild and your tests are negative for infections like the flu or strep throat, you might have one of hundreds of common cold viruses, which providers don’t often test for.
Treatment for upper respiratory infections depends on the cause. There aren’t any specific treatments for most viral URIs, like colds. Providers treat bacterial infections, like strep throat, with antibiotics.
Most viral URIs have to run their course and go away on their own. They usually last one to two weeks. You can ease your symptoms by drinking plenty of water and taking over-the-counter medications.
If you have a bacterial infection, your symptoms should start to improve a day or two after starting antibiotics. Don’t stop taking antibiotics even if you feel better — make sure you take the entire course as prescribed.
Upper respiratory infections caused by viruses are usually most contagious in the first few days of symptoms, and sometimes, a day or two before they start. But you could still be contagious even when you start to feel better, especially if you still have symptoms. Strep throat can be contagious for weeks if left untreated.
Contact a healthcare provider if your symptoms:
Long-lasting or frequent symptoms could be signs of a bacterial infection, fungal infection or other health condition. Talk to your healthcare provider if you have a compromised immune system or other health condition that might put you at higher risk for severe illness if you get an URI.
Advertisement
Go to the emergency room if you experience signs of severe illness, including:
You can reduce your risk of getting or spreading upper respiratory infections by:
Most of the time, no. Antibiotics don’t work on viruses, the cause of most URIs. You only need antibiotics if your provider diagnoses you with a bacterial infection, like strep throat.
The sore throat. The stuffy head. The seemingly endless runny nose. We all know that familiar upper respiratory infection (URI) feeling. Fortunately, most upper respiratory infections aren’t serious. But it doesn’t hurt to have a box of tissues, a humidifier and your favorite show or book at the ready for when one comes up. If you have any concerns about your symptoms, or you think you could have a bacterial infection, talk to a healthcare provider.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Need care fast? Cleveland Clinic’s Express Care and Urgent Care locations treat everything from sprains to sinus infections — no appointment needed.
