Ehlers-Danlos syndrome (EDS) is a genetic condition that weakens your body’s connective tissue. It commonly affects your skin and joints. There’s no cure, but your healthcare provider will help you find treatments to manage the symptoms and prevent dangerous complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
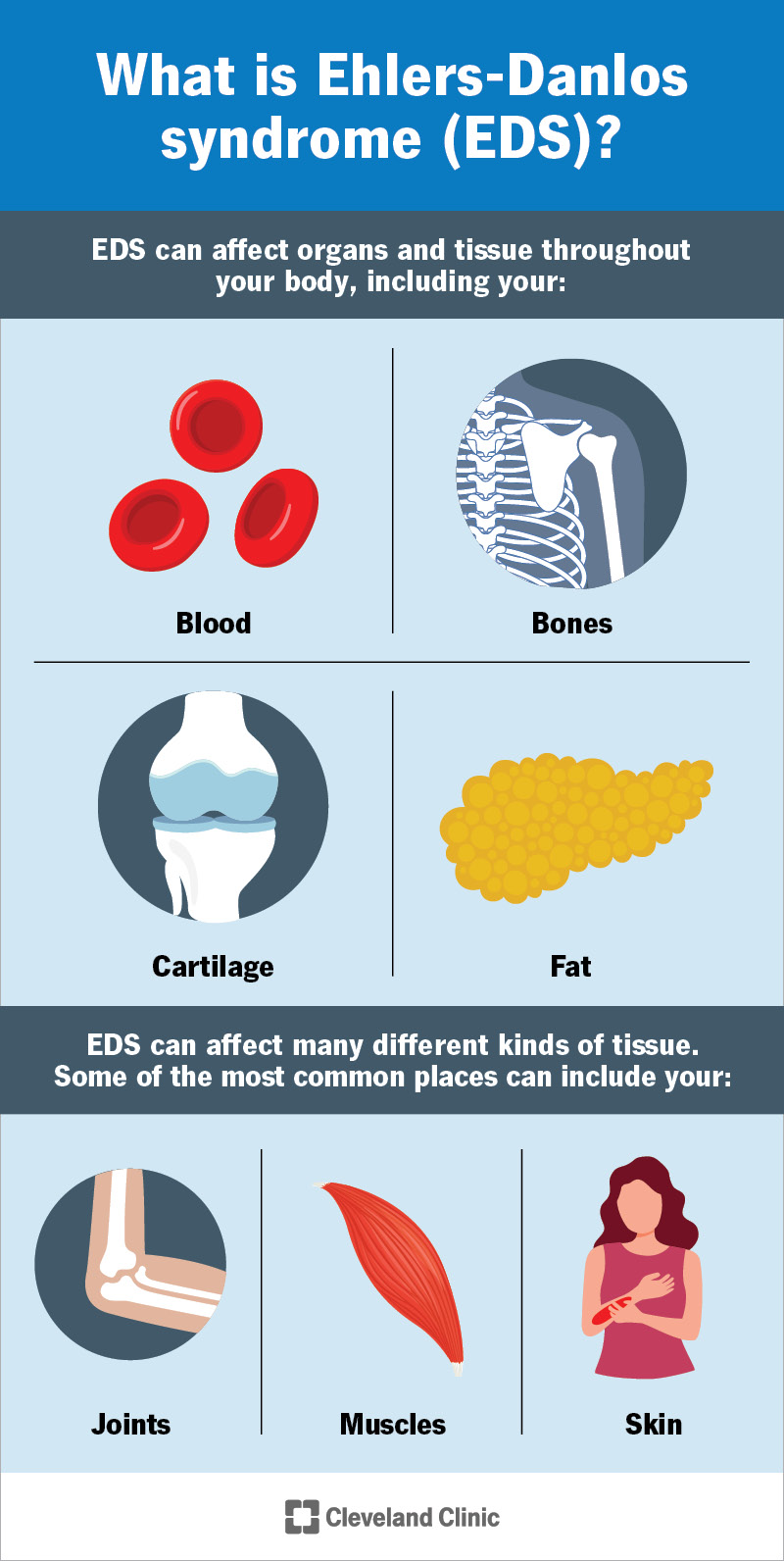
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/ehlers-danlos-syndrome-infographic)
Ehlers-Danlos syndrome (EDS) is a condition that affects the connective tissues in your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Connective tissues support your organs and hold parts of your body in place. They’re made of two proteins: collagen and elastin. Ehlers-Danlos syndrome makes your body produce weak collagen. This means your connective tissue can’t support you like it should. EDS can affect organs and tissue throughout your body, including your:
EDS can affect many different kinds of tissue. Some of the most common places can include your:
Healthcare providers classify EDS into 13 types based on where it affects you and the types of symptoms you experience. The five most common types include:
Advertisement
Symptoms can vary depending on which type you have. Some of the most common EDS symptoms include:
Ehlers-Danlos syndrome is a genetic condition. That means a genetic change causes it.
Experts have identified more than 20 different genetic changes that can cause EDS. They all affect your body’s ability to produce collagen. Which specific change you have determines which type you’ll develop and where it will affect you.
Some types of EDS are inheritable. This means biological parents can pass the genetic changes that cause it to their children. Other types happen randomly (somatically) and can’t be passed through generations of a biological family.
You may have an increased risk of Ehlers-Danlos syndrome if one or both of your biological parents have it. Similarly, if you have EDS, you might pass it to your biological children.
Talk to a healthcare provider about your risk of inheriting or passing EDS in your biological family. Your provider might suggest genetic counseling.
Dislocations are the most common Ehlers-Danlos syndrome complication. Never try to push a joint back into place on your own if you think you have a dislocation. Go to the emergency room (ER) right away.
Some types of EDS can cause life-threatening complications. For example, vascular EDS can make your blood vessels rupture (tear). This can lead to dangerous internal bleeding and stroke.
Advertisement
Your risk of complications depends on which type of Ehlers-Danlos syndrome you have. Other complications can include:
A healthcare provider will diagnose EDS with a physical exam and by discussing your medical history. They’ll examine your skin and joints and ask you about the symptoms you’re experiencing. Tell your provider when you first noticed symptoms and if anything makes them worse.
Your healthcare provider will suggest treatments for EDS that manage symptoms and prevent complications. Some common Ehlers-Danlos syndrome treatments include:
Your provider might suggest you avoid certain intense physical activities, like:
This can help you reduce the chances of experiencing a dislocation. You can still exercise and be active, but you may need to tweak or modify some activities to protect your joints.
Visit a healthcare provider if you notice any changes in your body that make your skin or joints feel weak or loose. See your provider if you notice that you’re bruising or bleeding more often than you used to.
Advertisement
Your provider will tell you how often you’ll need follow-up visits to track any changes in your body. They’ll help you change your treatments as needed.
You should expect to manage Ehlers-Danlos syndrome for the rest of your life. There’s no cure. But you should be able to participate in all your normal activities once you learn how to manage the symptoms.
EDS affects everyone differently. What you experience depends on which type you have and how it affects your body. Ask your provider what to expect based on your unique situation.
Living with Ehlers-Danlos syndrome can be hard work. It’s OK to feel frustrated sometimes. But try to give yourself credit, too, even for small wins. You deserve to feel safe and confident in your daily routine and during your favorite activities. And you should be able to once you learn to make any modifications you might need.
Don’t be afraid to ask questions or talk to your provider. EDS can cause subtle symptoms, especially at first. Trust yourself and trust your body. Talk to your provider if you feel like the symptoms are changing or your treatments aren’t working as well as they should.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have an inflammatory or autoimmune condition, you need experts by your side. At Cleveland Clinic, we’ll create an individualized treatment plan for you.
