
Breona Church had decided to name the daughter she was carrying “Journee” to signify her challenging pregnancy journey. It culminated in December 2022, when Breona was seven months pregnant and fainted at work, in her new job as a nurse.
Doctors discovered Breona had complications from Wolff-Parkinson-White (WPW) syndrome, a congenital heart condition that causes episodes of rapid heartbeats. While WPW can be controlled by medication in some cases, it can effectively be cured by undergoing catheter ablation, a minimally invasive procedure in which a thin tube is inserted into the heart to destroy abnormal tissue causing arrhythmia.

Breona during a follow-up appointment with Dr. Aziz at Cleveland Clinic. (Courtesy: Cleveland Clinic)
Traditional forms of catheter ablation require the use of X-ray fluoroscopy to guide the physician to the proper location within the heart. Since it’s best to avoid the use of X-rays where the unborn baby may be exposed to direct radiation, Breona’s cardiology team discussed the best path forward.
Options included closely monitoring her situation or administering medications to control the condition. However, Breona was hoping to take a more curative approach. “I didn’t want to be at home with my children, or driving, and have to worry about if I was going to pass out again,” recalls Breona, who also has a 5-year-old son, Abreon, and 3-year-old stepson, Jahad. “I’m the type of person who wants to get things taken care of, and I had faith my doctors could do it.”

Breona's son Abreon and Journee. (Courtesy: Cleveland Clinic)
Ultimately, Breona and her doctors agreed on a newer form of catheter ablation that uses 3D modeling rather than fluoroscopy, a procedure that is common in pediatric patients with heart rhythm abnormalities but has yet to gain widespread adoption for treatment with adults. According to Cleveland Clinic Children’s pediatric electrophysiologist Peter Aziz, MD, who collaborated with electrophysiologist Mohamed Kanj, MD, the technique eliminates the risks associated with radiology for both the patient who is pregnant and unborn child.
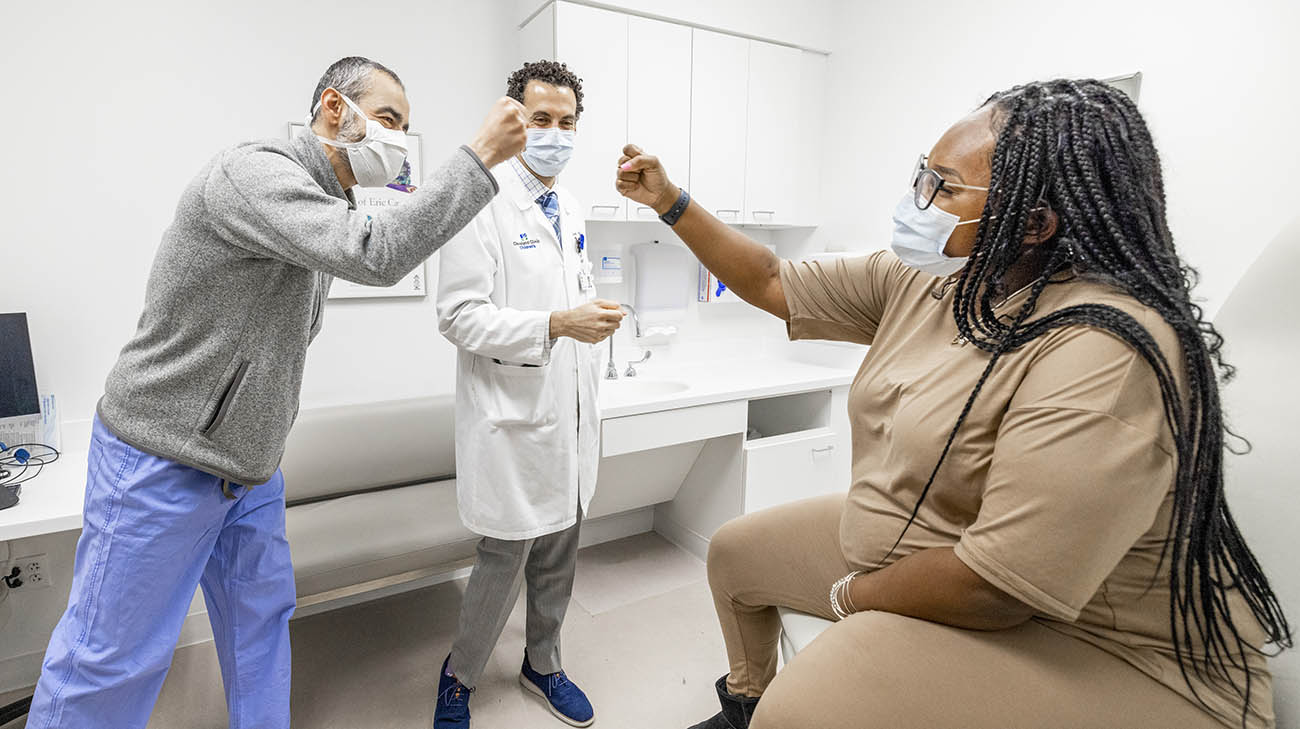
Breona with Drs. Aziz and Kanj after a follow-up appointment at Cleveland Clinic. (Courtesy: Cleveland Clinic)
“For most patients, we can take our time during the ablation,” explains Dr. Aziz. “But we don’t want to use anesthesia for too long in a patient who is pregnant. We’re trying to protect both the mom and fetus from any X-ray exposure, while expediting the procedure. Using 3D modeling was our safest and most effective option.”
Just a few days after her fainting spell, Dr. Kanj successfully performed the ablation using 3D modeling. While Breona will be monitored regularly in the future, 95% of patients who undergo a catheter ablation do not have a recurrence of their heart condition and require no further treatment, says Dr. Aziz.

Breona delivered Journee six weeks after she underwent an ablation where doctors used 3D modeling. (Courtesy: Cleveland Clinic)
Breona recovered quickly from the procedure and returned to work shortly after. Six weeks later, with the Maternal-Fetal Medicine team on alert, Breona was induced and delivered healthy baby Journee without incident. Journee shares the same birth date as Breona’s mom.

Breona is enjoying time at home with Journee and her family. (Courtesy: Cleveland Clinic)
Breona continues enjoying time spent bonding with her baby and family. “That pregnancy was a challenge from day one,” adds Breona. “But everything turned out great. I was definitely in the right place, at the right time.”
Related Institutes: Cleveland Clinic Children's , Heart, Vascular & Thoracic Institute (Miller Family), Ob/Gyn & Women's Health Institute

