
Parents Carolina Gonzalez and Sergio Serna say their lively daughter, Nicole, has always been an active and happy-go-lucky kid. Big sister and role model to 7-year-old brother, Max, mom and dad agree Nicole has always been more mature for her age, in part because of the challenges she faced at birth.
Born with unilateral congenital facial paralysis, Nicole, now 11, was unable to move the right side of her face, which drooped significantly compared to her left side. Unable to smile, or even completely close her right eye, Nicole couldn’t use her face to express emotion in conventional ways.

Nicole was born with unilateral congenital facial paralysis. The condition didn't allow her to move the right side of her face. (Courtesy: Carolina Gonzalez)
She underwent a pioneering, 12-hour facial reanimation operation performed in June 2021 by a team lead by Patrick Byrne, MD, Chairman of Cleveland Clinic’s Head & Neck Institute . Nicole was the first pediatric patient at Cleveland Clinic to undergo the complex procedure Dr. Byrne has been refining for years called a tri-vector gracilis free tissue transfer .
According to Dr. Byrne, who first examined Nicole in 2018 before coming to Cleveland Clinic in 2020, facial reanimation surgery can restore movement, function and symmetry to a patient’s face. This procedure can revitalize a person’s ability to talk, chew, drink and smile.
“Someone who is unable to express happiness or other emotions on their face often really struggles with their self-image because others are distracted by their face,” he explains. “Patients with facial paralysis are at much higher risk of depression. Restoring the ability to smile has incredible effects in improving a person’s mood and confidence.”

When considering the surgery for Nicole, Carolina and Sergio wanted to give her the best quality of life possible, while protecting and keeping her safe. (Courtesy: Cleveland Clinic)
Nevertheless, Carolina and Sergio labored over the decision to encourage their daughter to undergo facial reanimation surgery. “I loved her smile before the surgery, and I love her smile now,” says Carolina. “But I didn't want her to have to explain herself over and over again throughout her life about why she's different. We want her to be able to live her life to the fullest.”
Adds Sergio, “How do you explain to a kid she’s perfect the way she is but we want to do this procedure for her? It’s hard. There was a lot of crying, a lot of hugging.”
The decision was made easier by the couple’s trust in Dr. Byrne, which they immediately felt upon their initial meeting with him in 2018. “When we did the first consultation, we could tell he really cares for his patients,” recalls Carolina. “I am amazed by the kind of surgeon he is, but I am mostly amazed also by the human being he is.”
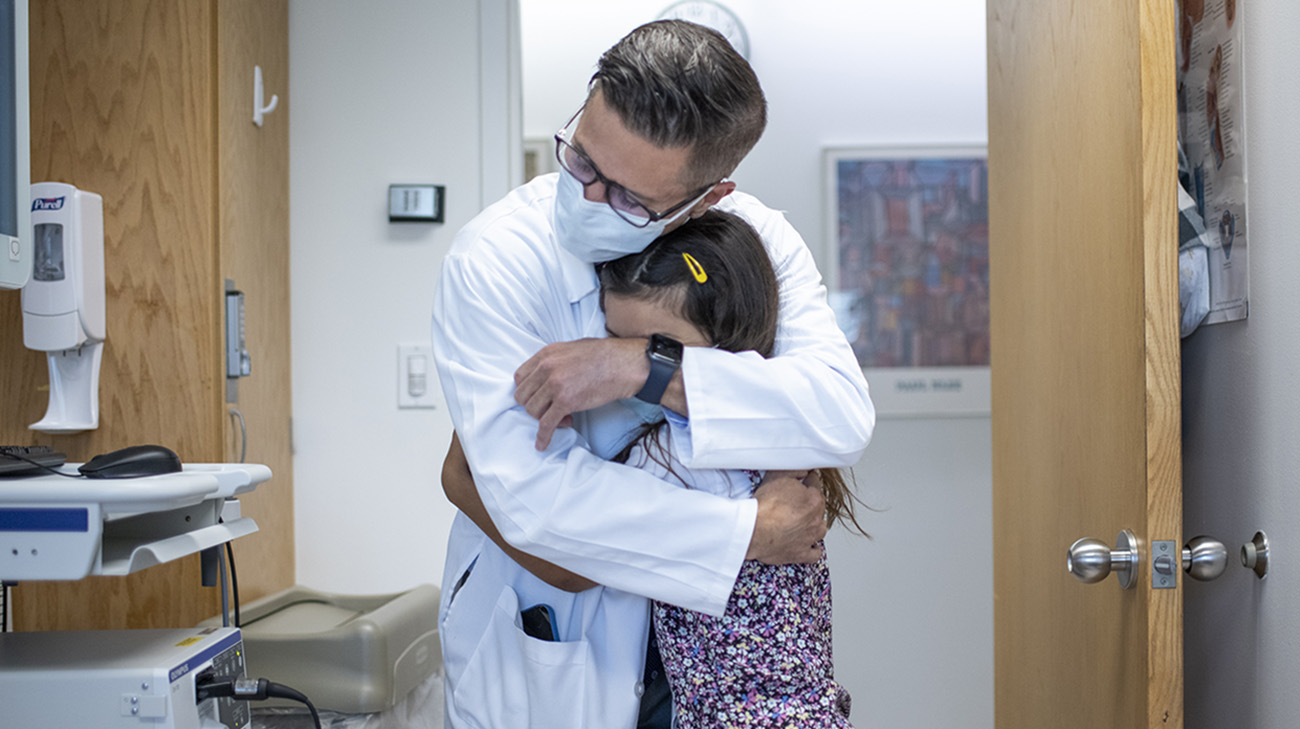
Carolina, Sergio and Nicole have always felt a great amount of trust in Dr. Byrne. Carolina says it's given her peace of mind to hear Dr. Byrne speak so passionately about caring for and treating patients. (Courtesy: Cleveland Clinic)
Congenital facial paralysis is quite rare, but surgeons throughout the world have treated it in recent decades, primarily through a procedure called microvascular free tissue transfer. It involves removing a single muscle or nerve from another area of the body and then implanting it into the face, typically near the mouth.
It has traditionally been performed as a single-vector procedure. In recent years, Dr. Byrne and colleagues modified and expanded the surgery to include transferring multiple slips of muscle. The purpose of these innovations was to create a more natural-looking smile, in which teeth show, therefore creating a “multi-vector” solution. While this procedure can be extremely beneficial, it has always excluded reanimating the area around the eye. As a result, there was a gap left in outcomes worldwide, considering people smile not only with their mouth but also their eyes. This led to the most recent innovation Dr. Byrne and the team have introduced. In Nicole’s case, they used a tri-vector approach to make her reconstructed smile even more natural, with muscles and nerves added to her mid-face and eye areas, in addition to her mouth.
The tri-vector gracilis free tissue transfer procedure includes harvesting the sural nerve from Nicole's lower leg for the cross-facial nerve graft and harvesting the gracilis free flap from her thigh. The rest of the surgery is performed in collaboration to carefully position and secure the flap, using microsurgical techniques to reconstruct the blood vessels and nerves. (Courtesy: Cleveland Clinic)
Notes Dr. Byrne, “While Nicole’s operation would be unique, we do microvascular free tissue transfers all the time, and that’s reassuring to parents. To entrust us to perform a big operation like this really takes a lot of faith. Nicole's parents are special, very thoughtful, and they really balanced their priorities for her – to be proactive and aggressive to help their daughter, while also ensuring they protect and keep her safe."

Nicole during a presurgery appointment with Dr. Byrne. (Courtesy: Cleveland Clinic)
In the days leading up to the surgery, the family of four travelled early from their home in Harrisonburg, Virginia, to Cleveland, Ohio, in order get settled and enjoy their surroundings before what they knew would be a long day. Trips to local Cleveland attractions proved to be fun-filled distractions.
One of Nicole’s happiest moments occurred the night before the surgery, back in their hotel room, when she, Max, Carolina and Sergio whirled and danced in the dark to some of Nicole’s favorite songs, their movements illuminated by waving bright, multicolored glow sticks.

Nicole, Carolina and Sergio in pre-op, moments before the clinical staff took Nicole to the operating room. (Courtesy: Cleveland Clinic)
“We had a dance party. It was so fun!” says Nicole. “We were just dancing around, enjoying ourselves, it was really cool.”
“Looking back, that party meant so much,” Carolina says. “For however long it lasted, it was a break in the tension we were feeling. Inside you have so many emotions going on, but you have to be the strong parent who gives your child that place of happiness and security.”
The day of surgery, as Dr. Byrne and his team began the intricate procedure, Nicole’s parents waited patiently, reassuring themselves this was the best decision for their daughter. First, the team closely examined the left side of Nicole’s face, determining exactly how her functioning facial and eye muscles were positioned. They then marked the right side of her face to map out exactly where her transplanted muscles should go.

Dr. Byrne marks Nicole's face in pre-op as part of presurgical planning. (Courtesy: Cleveland Clinic)
Next, the team disconnected a selected functioning facial nerve branch on the left side of Nicole’s face and reconnected it to the sural nerve that had been removed from the back of her left leg. They then placed it across her face, from one side (the functioning left side) to the other (paralyzed right side). Once those nerves were connected via a cross-facial nerve graft, a pathway existed so spontaneous smile-like movements on the left side would elicit movement on the right, too.
Then the team harvested the gracilis free flap, a band of muscles, from Nicole’s left thigh. They parsed the flap into thirds and inserted each segment into her face – one near her lip to help with a teeth-baring smile, one near the corner of her mouth to allow for a broad smile and one near her right eye to enable squinting near the corners. They also identified the “masseteric” nerve – a cranial nerve responsible for chewing – and rerouted part of it, from the base of the skull, to the implanted muscle bellies, to provide an additional power supply to drive facial movement.

Dr. Byrne and a multidisciplinary team of specialists, pediatric anesthesiologists and nurses completed Nicole's 12-hour facial reanimation procedure in June 2021. (Courtesy: Cleveland Clinic)
Finally, Dr. Byrne and the multidisciplinary team of nurses, pediatric anesthesiologists and a bevy of specialists, including Dane Genther, MD, a facial plastic and reconstructive surgeon and Brandon Hopkins, MD, a Cleveland Clinic Children’s pediatric head and neck surgeon, carefully reconnected every muscle, blood vessel and nerve.
“It couldn't have gone more smoothly. We got a beautiful reconstruction with very healthy blood supply and very solid motor nerve input,” states Dr. Byrne, who was inspired by Nicole for offering encouragement to a fellow patient facing a similar procedure, just days after her own surgery. “Nicole was a rock star. She managed any stress related to the surgery unbelievably well and bounced back really quickly.”
Nicole went home after four days in the hospital. After recovering from the surgery, she began the work of optimizing the impact of the procedure. Because she never previously had functioning muscles in the paralyzed areas of her face, she had to learn how to use them.

Nicole during a therapy session with Cleveland Clinic physical therapist, Mike Harrington. Nicole learns exercises to practice at home to increase muscle strength and regain facial coordination. (Courtesy: Cleveland Clinic)
“Nicole is in an age range in which she’s old enough to really engage in facial retraining efforts,” Dr. Genther explains. “After the surgery, physical therapists have to coach her on how to use the muscles. It’s a process that continues and improves for years.”
As the days and weeks passed, and Nicole’s facial swelling diminished, her parents noticed improvement in her facial symmetry. However, truly being able to produce what is known as a Duchenne smile – considered the most natural smile, as it includes a wrinkling in the eyelids’ corners – would take a lot of practice.

Nicole during a one-year postoperative follow-up appointment with Dr. Byrne at Cleveland Clinic. (Courtesy: Cleveland Clinic)
Besides countless physical therapy sessions, Sergio would implore Nicole to clench her mouth, something she had never been able to do beforehand. Finally, weeks into her recovery while she was at home, he and Max noticed some flickers of movement in her eyelids and the corners of her mouth.
Excitedly, the three of them found Carolina at home, to share the good news. Now, with each passing week, Nicole’s clenching and smiling ability continues to improve.

Nicole, Carolina, Sergio and Nicole's brother, Max, one year after Nicole's surgery. (Courtesy: Cleveland Clinic)
“We know from other cases the improvement we see at about one year out will continue for at least three or four more years,” states Dr. Byrne. “Especially at Nicole’s age, we see continued growth of the nerves and muscles into the face. The movements become more and more natural-appearing and symmetric.”
“It’s been a long journey, but we’re so grateful for it,” says Sergio. “We have peace knowing we did everything we could to give Nicole the best chance in doing whatever she wants in life.”
Related Institutes: Dermatology & Plastic Surgery Institute, Head & Neck Institute, Cleveland Clinic Children's , Anesthesiology & Pain Management

