
Watch and wait. That’s typically the prescribed procedure when a computed tomography (CT) scan detects small-sized nodules or lesions in the lung that may or may not be cancerous. Get annual CT scans, monitor any progression in shape or size, and then take proactive steps – such as lobectomy (partial removal of the lung), radiation or chemotherapy – should the growth develop into cancer.
That just wasn’t an option for 70-year-old David Sherman, a prominent Westlake-based attorney. Having successfully battled prostate cancer, he had also seen both of his parents die from lung cancer. So, although he was a nonsmoker, David was eager to end the suspense as soon as possible.
“Never in my life did I ever think I could get lung cancer. I never even touched a cigarette,” explained David. “But when they found the lesions, I wanted to know if I had gotten cancer. And if I did, I wanted to get it out of me before it spread.”
And that’s exactly what happened, thanks to an innovative procedure performed at Cleveland Clinic – a procedure performed by specialists at only a handful of other medical centers in the United States.
Using one of Cleveland Clinic’s hybrid operating rooms, a team led by thoracic surgeon Daniel Raymond, MD, and thoracic radiologist Jason Lempel, MD, performed a complex yet minimally-invasive technique – microcoil localization – to pinpoint and remove David’s tiny nodules without damaging additional healthy tissue.
“Rather than cutting out an entire lobe, or potentially even an entire lung, we can just take out a small bit of tissue,” explained Dr. Lempel. “So, we’re able to treat patients with early-stage lung cancers quickly and thus decrease the chance of the cancer spreading.”
The two-stage procedure typically proceeds in the following manner: After the patient goes to sleep in the operating room, a radiologist - using the hybrid operating room CT scanner and its advanced software capabilities - inserts a needle pre-loaded with a soft, fiber-coated platinum thread through the chest wall, then through the lung and finally, into the target nodule. This coil is carefully anchored to the nodule before the needle is removed.
A radiologist inserts a needle into the lung and target nodule. (Courtesy: Cleveland Clinic)
Then, a thoracic surgeon – using video-assisted thoracoscopic technology (VATS) – locates the coil on the pleural (membrane around the lungs) surface, and carefully removes it along with the wedge of tissue containing the small nodule or lesion. Then, the team can instantly examine the tissue, make a diagnosis and perform further surgical treatment, if necessary.
A thoracic surgeon locates the coil and resects the wedge of tissue containing the small nodule. (Courtesy: Cleveland Clinic)
Dr. Raymond is optimistic that microcoil localization may one day vastly reduce the need for lobectomy, a surgical procedure in which a much larger section of the lung tissue is removed.
“Eighty-five percent of lung cancer patients present with stage 4 disease, where the (cancer) has spread to the bone or brain,” he noted. “If we can detect these patients earlier with CT screening and use microcoil techniques to treat patients sooner, we’re going to be able to treat many more patients and save a lot of lives in the process.”
A review of the Cleveland Clinic team’s first 20 cases using microcoil localization revealed a 100 percent success rate in retrieving the target lesion with clear margins, meaning no cancer cells were detected at the outer edge of the removed tissue.
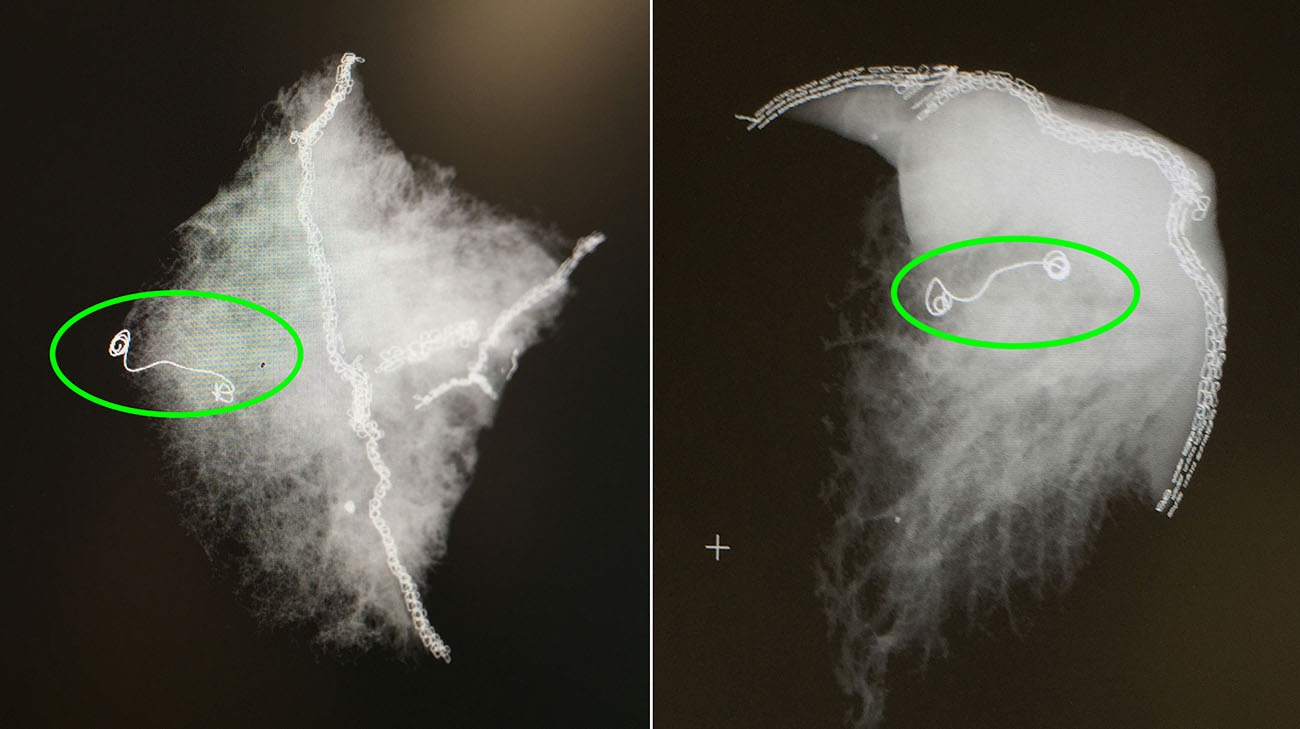
X-ray images of lung samples with the microcoil. (Courtesy: Cleveland Clinic)
In David’s case, the team discovered one of the nodules they removed was a very early stage lung cancer. With all the cancerous tissue removed at this early stage, doctors believe David has a 90 percent chance of survival over a five-year period.
“They found I had lung cancer, they took it out, and I never even had any pain,” recalled David. “Now, I have no trouble breathing. I’m good to go!”
Related Institutes: Cleveland Clinic Cancer Center, Respiratory Institute

