Brachytherapy for prostate cancer treats tumors with tiny radioactive implants placed in your prostate. Radiation oncologists may call the treatment permanent or low-dose-rate brachytherapy because the implants stay in your prostate. Prostate cancer brachytherapy is an effective treatment for cancer that hasn’t spread to other areas of your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
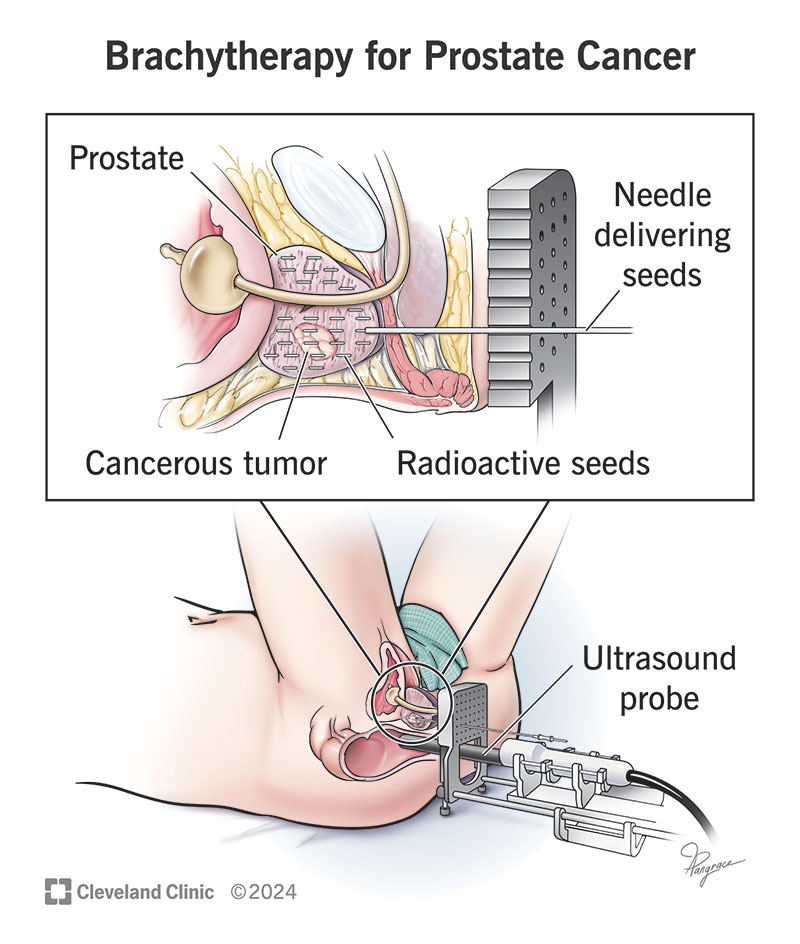
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/brachytherapy-prostate-cancer)
Brachytherapy for prostate cancer is a type of radiation therapy. It involves placing tiny, radioactive implants near cancerous tumors in your prostate. There are different types of prostate cancer brachytherapy. This article focuses on permanent (low-dose rate) brachytherapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In this treatment, implants release low doses of radiation over 10 to 12 months and then remain in your body. Radiation oncologists may use the term “seeds” or “capsules” when talking about the implants.
The pre-operative nursing staff will prepare you when you arrive. Your anesthesiologist will give you medication to make you relax and stay comfortable during the procedure.
Brachytherapy for prostate cancer is very successful, but everyone is different. One analysis of long-term success found that 97% of people who received permanent/low-dose-rate brachytherapy were alive 17 years after completing treatment.
Advertisement
That said, people who have this treatment should have regular prostate cancer screening tests. Your healthcare provider will recommend how often you should see them.
Low-dose rate brachytherapy targets cancerous prostate tumors and reduces the chance that radiation will harm nearby healthy tissue. This treatment causes fewer long-term complications and side effects than other types of radiation therapy.
Permanent/low-dose-rate brachytherapy may cause immediate, short-term and long-term side effects.
The treatment area may feel sore and swollen. You may notice bruising. These side effects are mild and go away within two or three days.
You’ll probably need to pee more often than usual or feel like you need to pee right away. There may also be a burning sensation when passing urine. These side effects usually become less noticeable over the next six to eight weeks.
You may have some slight bleeding. Contact your provider if you’re bleeding more than you expect or if you see large clots of blood in your pee.
The treatment may cause long-term side effects, including erectile dysfunction, radiation cystitis and radiation proctitis. Radiation exposure is another possible side effect.
Research suggests 25% of people who have this treatment develop erectile dysfunction (trouble maintaining an erection). It’s important to remember that prostate cancer typically affects people age 50 and older, and that people often live for many years after treatment. You could develop erectile dysfunction that’s not related to your prostate cancer treatment.
Radiation cystitis doesn’t happen very often. But you should contact your provider if you notice blood in your pee.
This condition is an uncommon complication. It affects less than 3% of people who have radiation in their pelvic areas, including the prostate. Radiation proctitis causes bleeding and inflammation in your rectum after radiation therapy.
The radioactive implants in your prostate will give off very small amounts of radiation. You may worry that you’ll spread radiation to other people, particularly small children or pregnant women.
It’s safe for them to be near you, but avoid letting them sit in your lap for extended periods. In general, it’s a good idea not to have a small child or pregnant woman sit on your lap for more than 20 minutes at a time for two months after your procedure. But everyone’s situation is different. Ask your radiation oncologist for guidance.
Most people can get back to their usual activity within one to two days after treatment. In general, it’s a good idea to take it easy and let your provider know if you’re having trouble with daily activities.
Avoid activities that put pressure on your groin — like horseback riding or cycling — for two months after treatment.
Advertisement
Contact your provider if your side effects don’t go away as soon as you expected or are more severe than you expected. You should also contact them if you notice new symptoms that could be signs that prostate cancer has come back.
If you’re considering brachytherapy for prostate cancer, know that you’re not alone — and you’re not expected to understand everything all at once. Brachytherapy uses tiny, radioactive seeds placed in or near your prostate tumor to target cancer directly. The seeds stay in your body and slowly release radiation over time. This treatment is safe and effective, and it may be a good option for you.
It’s normal to have questions or concerns. Your radiation oncology team is here to support you every step of the way — explaining what to expect, answering your questions and helping you feel confident in your care decisions.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
A prostate cancer diagnosis can change your life. At Cleveland Clinic, we can help you feel like yourself again with expert treatment and support.
