Radiation therapy, along with chemotherapy and surgery, is one of the most powerful tools we use to treat cancer. Radiation therapy includes the most common type, external beam radiation therapy (EBRT), and internal radiation therapy. Your radiation oncologist can recommend radiotherapy tailored to your condition and the kind of cancer you have.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
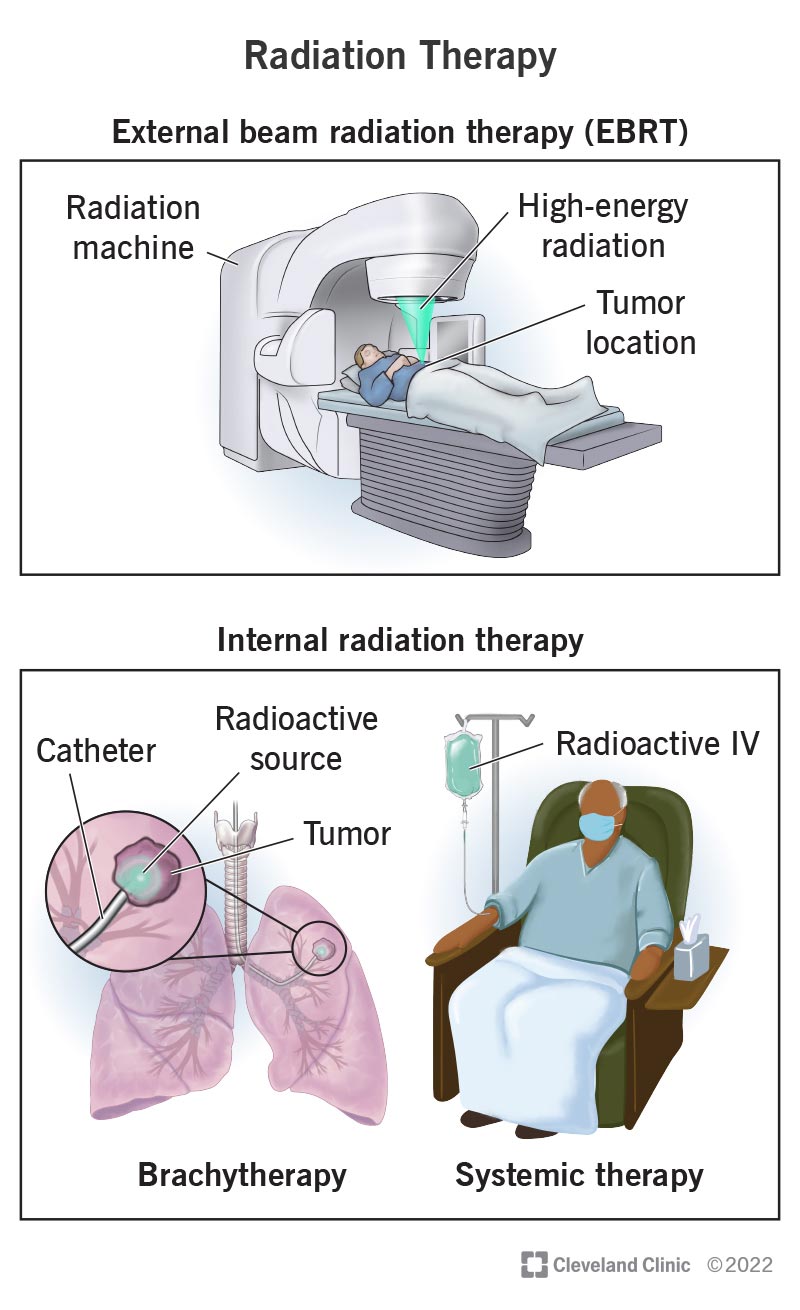
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/17637-radiation-therapy)
Radiation therapy — or radiotherapy — is a common cancer treatment that uses radiation (usually high-powered X-rays) to kill cancer cells. Radiation therapy may be used independently or alongside other treatments, like surgery or chemotherapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Radiation oncologists are healthcare providers who specialize in radiation therapy. Your radiation oncologist will determine whether radiation therapy would benefit you. If so, they’ll determine the best type of radiation therapy for the kind of cancer you have. They also design the radiation treatment plan with the radiation dosage that will destroy cancer cells without harming nearby healthy tissue.
There are two main types of radiation therapy: external beam radiation therapy (EBRT) and internal radiation therapy. Both types work by destroying a cancer cell’s DNA. Without DNA instructions telling them to grow and multiply, cancer cells die and tumors shrink.
External beam radiation therapy (EBRT) is the most common type of radiotherapy. With EBRT, a machine directs beams of high-energy radiation toward the tumor. The energy may be X-rays (most common), electrons or protons. Precision is vital with EBRT. Your radiation oncologist will design a treatment plan to target the tumor with radiation while avoiding your healthy tissue.
There are many forms of EBRT:
Advertisement
Internal radiation therapy places radiation inside of your body, close to cancer cells. It treats smaller tumors in your head, neck, breast, cervix, uterus or prostate.
You can receive internal radiation through a solid source or in liquid form:
Radiation therapy kills cancer cells, shrinks tumors and relieves cancer symptoms. It may be your only treatment, or it may be used to:
Radiation therapy can also destroy benign (noncancerous) tumors causing symptoms. In select cases, providers may also use low-dose radiation therapy to treat certain conditions.
For internal radiation therapy, you may need a physical exam and imaging. Your radiation oncologist will explain how you can prepare for the day of the procedure based on how you’ll receive the radiation.
External beam radiation therapy (EBRT) involves a planning appointment called a simulation. Simulation is the treatment planning step that customizes your treatment.
Simulation involves:
Simulation allows your radiation oncologist to determine your radiation dosage and how you’ll receive it.
Internal radiation therapy usually happens in a special outpatient treatment room or in a hospital. Your radiation oncologist may insert the radiation implant using a small flexible tube called a catheter. For this treatment, you’ll receive anesthesia so you don’t feel pain or discomfort during the procedure. With the systemic form of internal radiation therapy, you’ll receive radioactive fluid through an IV.
Advertisement
With EBRT, you lie on a table, positioned as during simulation. The radiation machine moves around you but never touches you. A healthcare provider called a radiation therapist operates the machine from a separate room. You can speak to each other at any time using an intercom. The machine directs precise doses of radiation toward the tumor as it shifts positions. You won’t feel anything during treatment.
With internal radiation therapy, you’ll typically go home after a short recovery the same day. Occasionally, you may need to stay in the hospital while your body sheds trace amounts of radiation. After systemic (IV) radiation therapy, you may secrete small amounts of radiation through body fluids, like sweat, pee and blood.
If you receive IV or permanent internal radiation therapy, there’s a small risk of exposing others to radiation. Follow your radiation therapy team’s guidance about how much contact you should have with others after radiotherapy.
You should be able to go about your regular daily activities before and after EBRT. There’s no risk of exposing others to radiation.
Most people receive radiation therapy spread out over multiple treatment sessions so they don’t receive the full dose all at once. The treatment schedule gives your healthy tissue time to recover between sessions. The healing time reduces side effects.
Advertisement
Still, you may experience unpleasant side effects that your radiation oncologist will help manage. Usually, these side effects only affect the part of your body receiving radiation directly.
Side effects may include:
Ask your radiation oncologist what side effects to expect, given the kind of radiation therapy recommended for the kind of cancer you have.
Radiation therapy is a reliable and effective cancer treatment that’s been around for over a century. Depending on the type of cancer you have, radiation therapy can destroy cancer cells and help other treatments work better. It’s also an important part of palliative care. It can ease cancer symptoms so that you live a fuller, more enjoyable life.
Although radiation therapy effectively treats many types of cancer, it may also increase your likelihood of developing a different cancer in the future. For many people, the benefits of radiation therapy are worth the risk.
Advertisement
Weigh the benefits of treatment against potential risks with your radiation oncologist.
Some people receiving radiation continue their routine with no problems. Others feel so sick that they need to take time out to rest. Many people don’t experience side effects until several weeks into treatment when more cells die.
Discuss best and worst-case scenarios with your radiation care provider as you plan your schedule around treatment.
Your radiation care provider should know about any side effects you’re experiencing, especially those that interfere with your quality of life. Depending on your treatment response, your provider may need to adjust your dosage, change your treatment schedule or try a different type of treatment.
If you have cancer and radiation therapy is one way to treat it, don’t hesitate to ask for specifics. Various forms of radiation therapy exist that can target specific cancers and tumor types. They allow radiation oncologists to deliver precise doses of radiation that can kill cancer cells while sparing healthy tissue. Ask how a particular form of radiotherapy will work to target the tumor while minimizing harmful radiation exposure.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic offers expert radiation oncology with advanced technology, personalized care and virtual visits to support you every step of the way.
