Epilepsy is a long-term condition that causes seizures due to unusual electrical activity in your brain. Seizures can look different for each person, from brief staring to shaking. While there isn’t a cure, treatments like medications, surgery and lifestyle changes may reduce symptoms and improve quality of life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Epilepsy is a long-term brain condition that causes repeated seizures. Seizures happen when there’s abnormal electrical activity in your brain. Symptoms can range from brief staring spells or confusion to strong shaking and temporary loss of consciousness.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Epilepsy can develop after a brain injury, stroke or tumor. But in many cases, the cause isn’t known.
About 50 million people worldwide have epilepsy. Anyone of any age, race or sex can develop this condition. A healthcare provider can help you manage it.
Healthcare providers often group epilepsy types based on where abnormal electrical activity starts in your brain. They’re similar to seizure types and include:
From here, your provider may give you a specific epilepsy or seizure type based on the lobe in your brain where seizures are, like temporal lobe epilepsy. Types may also focus on features specific to the seizure itself, like absence seizures, tonic–clonic seizures or febrile seizures, among others.
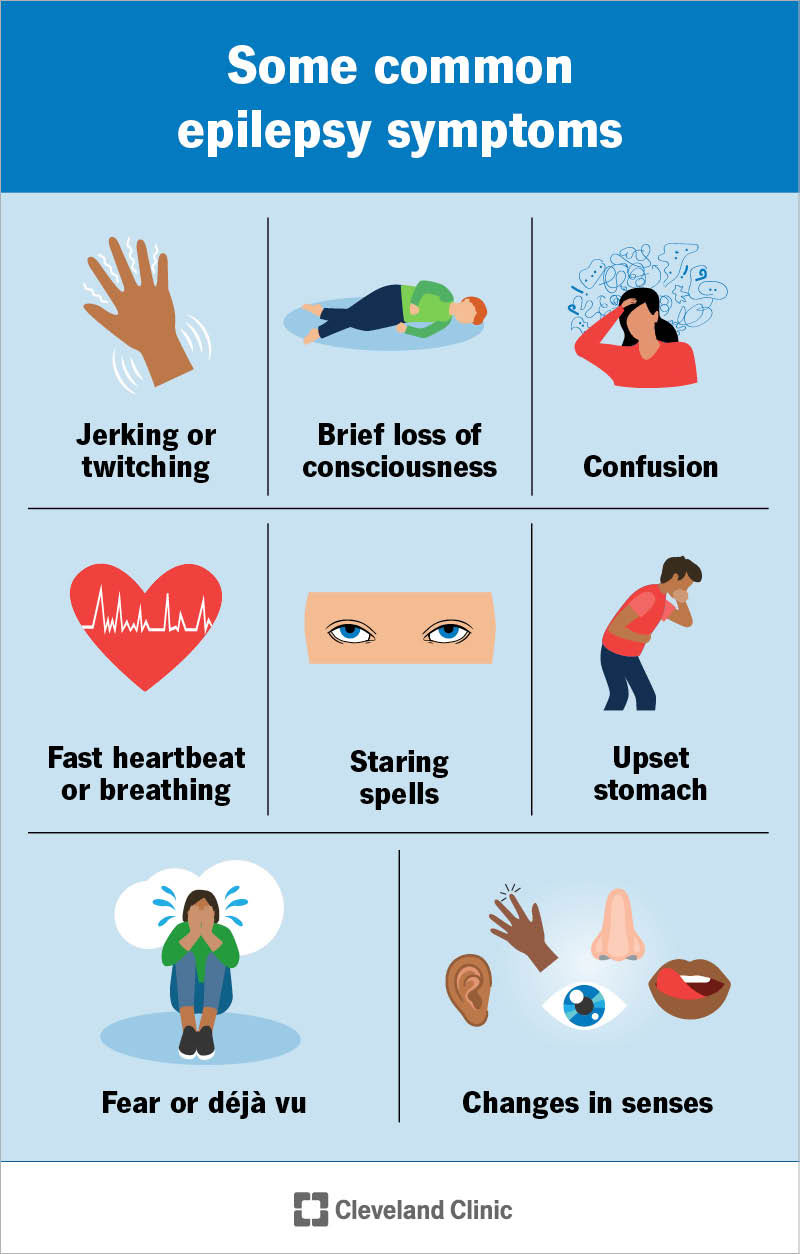
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/epilepsy)
The main symptom of epilepsy is repeated seizures. Symptoms can look different depending on the type of seizure. But many people have similar symptoms each time they have one.
Advertisement
Common symptoms include:
Abnormal electrical activity in your brain causes epilepsy. Your brain works by sending electrical signals between nerve cells. These signals help control how you think, feel, move and respond to the world around you.
In epilepsy, these signals don’t always send in an organized way. Instead, many brain cells fire all at once or much faster than they should. This sudden burst of electrical activity causes symptoms.
This condition can have many causes, and sometimes no clear one is found. Possible causes may include:
Epilepsy triggers are things that can make seizures more likely to happen. Common triggers may include:
You may also notice symptoms happen more often when you’re dehydrated or skipping meals. Triggers can vary from person to person, so learning what affects you may help you better manage this condition.
You may have a higher risk of developing epilepsy if you have:
Having one or more risk factors doesn’t mean you’ll develop epilepsy. But it may raise the likelihood.
Possible complications may include:
Advertisement
Some activities require your full attention and quick reactions, like driving, swimming alone, climbing or operating heavy equipment. These may not be 100% safe if you have epilepsy. Your healthcare provider can help you understand which activities are safe for you and what precautions you should take.
Serious medical complications may include:
You may get an epilepsy diagnosis if you have more than one seizure. This usually means:
Seizures caused by something short term, like illness, alcohol withdrawal or a recent head injury, don’t count toward an epilepsy diagnosis. But they may if there’s evidence your brain has an ongoing risk.
Advertisement
If you’ve had a seizure, your provider will likely refer you to a neurologist. One of the most important parts of diagnosis is describing what happened. Your provider will ask what you remember before, during and after the seizure.
But many people don’t remember what happened. So, it can help to bring someone who saw it or to have them write down or record what they noticed.
To confirm the diagnosis and rule out other conditions, your provider may order tests like:
Even if test results are normal, your doctor may still diagnose epilepsy based on your seizure history and symptoms.
There’s no cure for epilepsy. But there are many options to treat it. Your provider might recommend:
Advertisement
Your healthcare provider will help you choose the best option based on your seizure type, age and general health.
Visit the emergency room if you have a seizure for the first time. If others notice that you “zoned out” or briefly lost awareness, give a provider a call. They may refer you to a neurologist for further testing and care.
If you’re with someone who’s having a seizure that lasts longer than five minutes or has several seizures in a row without fully waking up in between, call 911 or your local emergency services number.
Epilepsy is a long-term condition that affects everyone differently. A healthcare provider can help you manage symptoms, but it may take a little time to find the perfect plan. You’ll need to see your healthcare provider regularly, and they may adjust your treatment plan over time.
Managing epilepsy often includes caring for your overall well-being. This not only includes your brain, but also your sleep, stress and mental health. Your care team can help you find what works best for you.
Not all cases of epilepsy can be prevented. But some steps may help lower the risk:
Living with epilepsy can bring a lot of unknowns. Whether it’s the unpredictability of seizures or the process of finding the right treatment, it’s normal to feel uncertain at times. But managing epilepsy isn’t just about stopping seizures — it’s also about creating a life where you feel safe, supported and in control.
There are many tools to help you get there, from medications to lifestyle changes and care teams that understand the condition inside and out. Over time, many people with epilepsy find routines that work for them.
If something doesn’t feel right or changes, your provider can help adjust your care and support you along the way.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Epilepsy and seizures can impact your life in challenging ways. Cleveland Clinic experts can help you manage them and find relief.
