Cochlear implants are electronic devices that reduce hearing loss. They don’t restore hearing. Instead, they improve your ability to understand speech and hear more sounds. Adults and children who receive cochlear implants benefit by having auditory therapy that helps them relearn how to hear.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
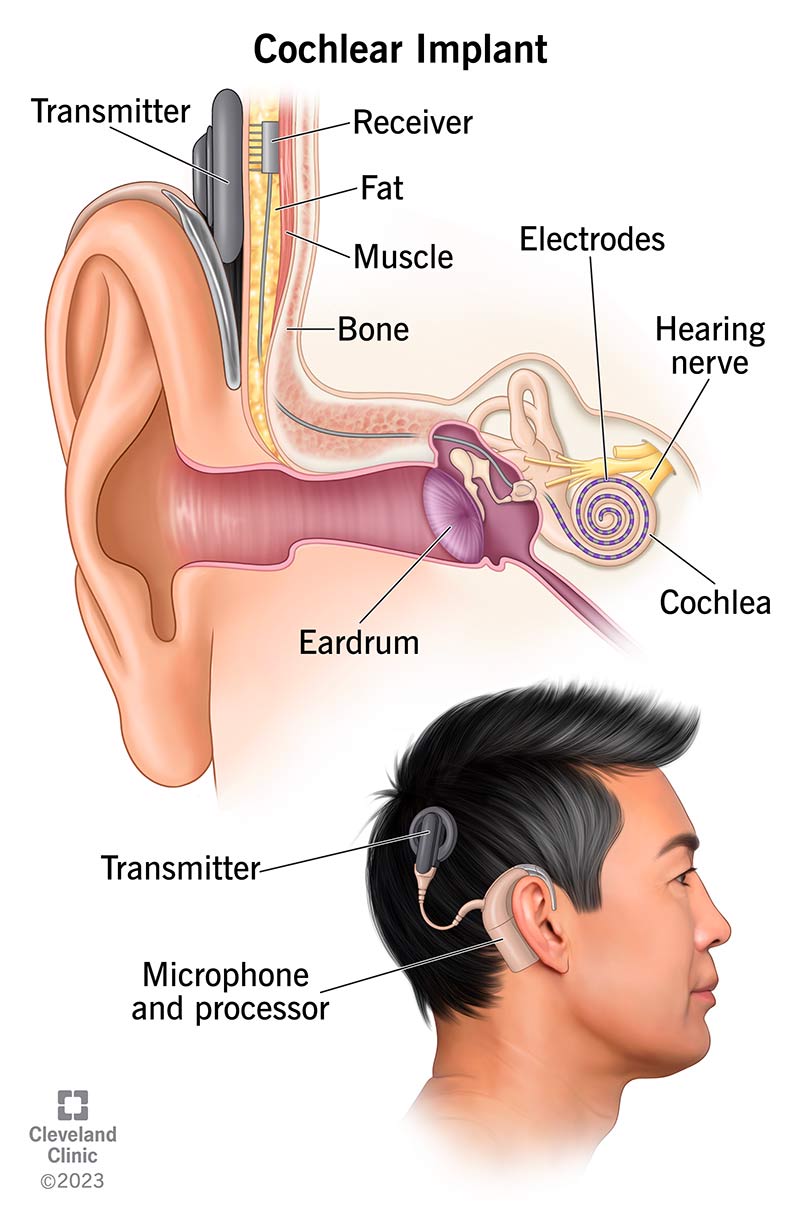
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/4806-cochlear-implant)
Cochlear implants are electronic devices that help manage hearing loss. Your healthcare provider may recommend this treatment if you have moderate, profound or severe hearing loss in one or both ears and you’re not benefiting from your hearing aids. You may also benefit from a cochlear implant if your hearing aids work, but you still can’t understand speech as well as you’d like.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cochlear implants don’t restore your hearing. But they can improve your ability to understand speech and hear other sounds.
All cochlear implants include an external part you wear and an internal part that a surgeon will place during surgery:
How you wear the external parts of the device depends on the type you get:
Unlike hearing aids, which turn the volume up on sounds, cochlear implants bypass damaged parts of your ear. Most hearing problems happen because of damaged sensory hair cells inside your cochlea (sensorineural hearing loss). Your cochlea is inside your inner ear, deep inside your skull. It changes sound signals that enter your ear into electrical impulses your brain interprets as sound.
Cochlear implants create a new pathway for sounds to reach your brain. It works like this:
Advertisement
Your brain perceives the electrical impulses as speech, music or other noise.
First, you’ll need cochlear implant surgery to place the internal parts. It’s an outpatient procedure, which means you can go home that same day. Your surgeon (an otolaryngologist) will:
About two weeks after surgery, you’ll have a follow-up appointment to put on the external parts. A hearing specialist (audiologist) will:
You’ll have your cochlear implant forever, so you’ll work with audiologists and surgeons for the rest of your life. You’ll have regular appointments so your care team can confirm that:
The benefits of cochlear implants far outweigh the risks. This is true whether you have complete hearing loss or if hearing aids help, but you want to hear better.
Here’s a snapshot of the benefits:
That said, all surgeries come with risks. Although they’re rare, risks specific to cochlear implant surgery include:
It may take some time before you notice a big change for the better. That’s because your brain needs to relearn how to process sounds. In general, people’s hearing improves about a month after their implants are activated. Sometimes, it takes three to six months for people to reach their full hearing potential.
Advertisement
In the meantime, you’ll likely work with an audiologist or a speech-language pathologist (SLP). They can help train your brain to understand what sounds mean. You need to be committed to doing auditory-based therapy to get the most out of your implant.
Adults who get cochlear implants often say that speech sounds mechanical at first. But eventually, the sounds from your cochlear implant will become natural. In general, the earlier in life you get an implant, the easier it is to adapt to the new way of hearing.
Still, the learning curve depends a lot on the type of hearing loss you have and how severe it is. The time you devote to therapy matters, too.
To get the most out of this treatment:
Advertisement
Contact your provider if you notice hearing changes or you have ear pain or discomfort in your ears. Let them know immediately if you or your child has signs of an infection, like a fever and redness, swelling or drainage at the surgery site.
It depends. A cochlear implant can’t help you hear as you would without inner ear damage. But it can help you access sounds that can help with understanding what others are saying. It can help you perceive noises in your surroundings that alert you to danger. Working with an audiologist or SLP can give you the tools you need to get the most out of your implant.
Not always. Historically, you could expect to lose all hearing after cochlear implant surgery. But improved cochlear implant surgery techniques and implant design mean that about half of people retain their hearing after surgery.
A cochlear implant can be life-changing. If you have hearing loss, it may be a way back to a world you thought you’d never hear again. If your child was born with hearing loss, a cochlear implant could be their first step into a world of sounds. But cochlear implant surgery is just the beginning. You or your child may need hearing rehabilitation therapy to relearn how to process sound. The journey may take some time. But your hearing team will be with you every step of the way.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cochlear implants can help your child hear better and communicate with the world around them. Cleveland Clinic Children’s is here to bring sound to their life.
