Paracentesis is a procedure that removes fluid buildup inside your abdomen, called ascites. Your healthcare provider may remove a small amount of fluid to test for what’s causing the buildup. Or, you may need paracentesis to relieve symptoms of ascites, like pressure and pain in your abdomen.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
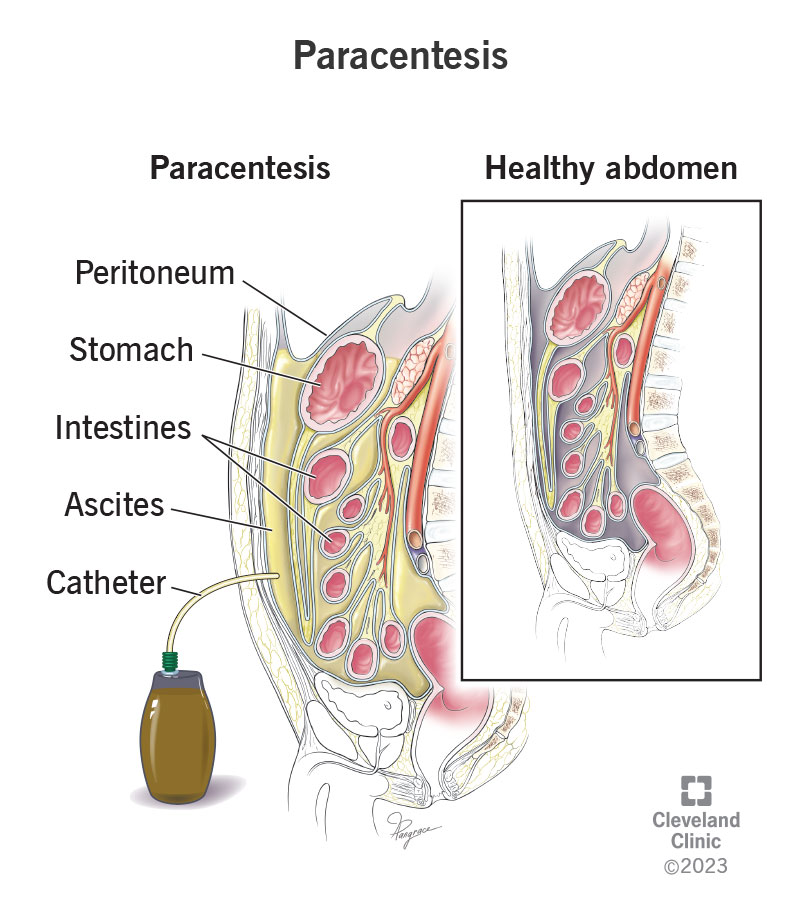
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/paracentesis.jpg)
Paracentesis is a procedure that drains excess fluid called ascites from your abdomen. Ascites occur when fluid collects in a membrane called your peritoneum. Your peritoneum covers your abdominal organs, including your stomach, liver, kidney and parts of your intestines. It consists of two layers. Ascites form when fluid builds up between the two layers, a place called your peritoneal cavity.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
During paracentesis, a healthcare provider uses a needle and a plastic tube called a catheter to drain the ascites. Draining the fluid can relieve unpleasant symptoms like pressure in your abdomen. Sometimes healthcare providers drain the fluid to run tests on it. Test results show what’s causing ascites.
Healthcare providers perform paracentesis to diagnose conditions that cause ascites. Paracentesis is also a treatment. Your provider may recommend paracentesis if more conservative treatments for ascites, like water pills (diuretics) or switching to a low-sodium diet, haven’t helped.
Paracentesis can help your provider diagnose common causes of ascites, including:
Therapeutic paracentesis can relieve symptoms of ascites. Common symptoms include:
Advertisement
Your healthcare provider will explain the procedure and ensure you’re prepared. They’ll:
You can get paracentesis in your provider’s office or at a hospital. You may need to pee beforehand so your bladder is empty for the procedure.
Once you’re ready, a healthcare provider will:
If ascites frequently return after paracentesis, your provider may place a tube called a tunneled peritoneal drainage catheter into the drainage site. You’ll wear this tube long-term, so you won’t have to keep returning for paracentesis. Part of the tube goes inside your abdomen, and the other side goes outside. The outside part attaches to a bottle that continually collects fluid. You’ll drain the bottle at home.
Advertisement
Your healthcare provider will advise you on whether this is a good option.
Paracentesis takes from 20 to 45 minutes. Timing depends on how much fluid is removed.
For diagnostic paracentesis, your healthcare provider will remove enough fluid to perform all the necessary tests. This is usually about 25 milliliters (ml).
For therapeutic paracentesis, the amount of fluid depends on how much excess fluid you have and whether you have a history of fluid returning. Often, removing 5 liters is enough to relieve abdominal pressure from ascites. Your provider may remove more fluid if your ascites often return (recur).
You may feel a brief sting when the numbing needle goes in. You may also feel pressure or discomfort during the draining, but it shouldn’t feel painful.
Still, let your provider know if you feel uncomfortable or light-headed during the procedure. This is more likely to happen if your provider removes large amounts of fluid. They can give you pain medicines that can help.
Your care team will monitor your vital signs for about an hour afterward. While you’re recovering, you may notice small amounts of clear fluid seeping from the bandaged site, but don’t be alarmed. This is normal.
If the procedure is diagnostic, your provider will send the fluid sample to a lab for peritoneal fluid analysis. The analysis includes a series of tests that may include any of the following:
Advertisement
Tests may also check your levels of:
Knowing these levels can help your healthcare provider determine if your ascites likely result from cancer, an infection, an injury to an organ (like your bowel), organ damage (like heart failure) or other common causes.
Paracentesis can relieve symptoms of ascites and help your healthcare provider determine what’s causing fluid to build up.
Paracentesis can save your life, depending on your circumstances. Studies have shown that people with ascites related to cirrhosis who are admitted to the hospital live longer if they have paracentesis. People with bacterial peritonitis (a common infection associated with ascites) who have paracentesis receive life-saving antibiotics sooner than they would have had they not had the procedure.
Advertisement
The fluid does return for some people. Depending on your condition, you may only need paracentesis once to get rid of the ascites. Other people have to return as often as every few weeks.
Your healthcare provider can advise you on how often you’ll need paracentesis based on your condition.
Complications with paracentesis are rare, but they can happen. Complications include:
Resting the first 24 hours after your procedure is a good idea. It may take a day or two for small amounts of fluid to stop seeping from the drainage site. But your body should recover quickly.
Follow your provider’s guidance on when it’s safe to resume normal activities based on your lifestyle.
Your healthcare provider will instruct you on caring for the wound. You may also need to adjust what you eat and drink. They’ll advise you on:
Contact your healthcare provider if you notice any signs of a complication, including bleeding from the site or an infection. Signs of an infection include:
Visit the ER if you have:
Paracentesis is a low-risk procedure that can help your healthcare provider diagnose what’s causing fluid buildup in your abdomen. It can also help relieve symptoms if you’re living with a condition causing ascites. Paracentesis may be a one-time procedure, depending on your condition, or you may need it frequently. Your provider may need to remove a small amount of fluid if they’re trying to diagnose a condition but a larger amount if you have recurring ascites. Ask about what factors will shape your experience before going in for paracentesis so you know what to expect.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have issues with your digestive system, you need a team of experts you can trust. Our gastroenterology specialists at Cleveland Clinic can help.
