Mast cell activation syndrome (MCAS) is a condition that causes intense episodes of swelling, shortness of breath, hives, diarrhea, vomiting and other symptoms. In severe cases, it may lead to life-threatening anaphylaxis. It’s caused by mast cells (mistakenly) alerting your immune system that there’s something harmful in your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
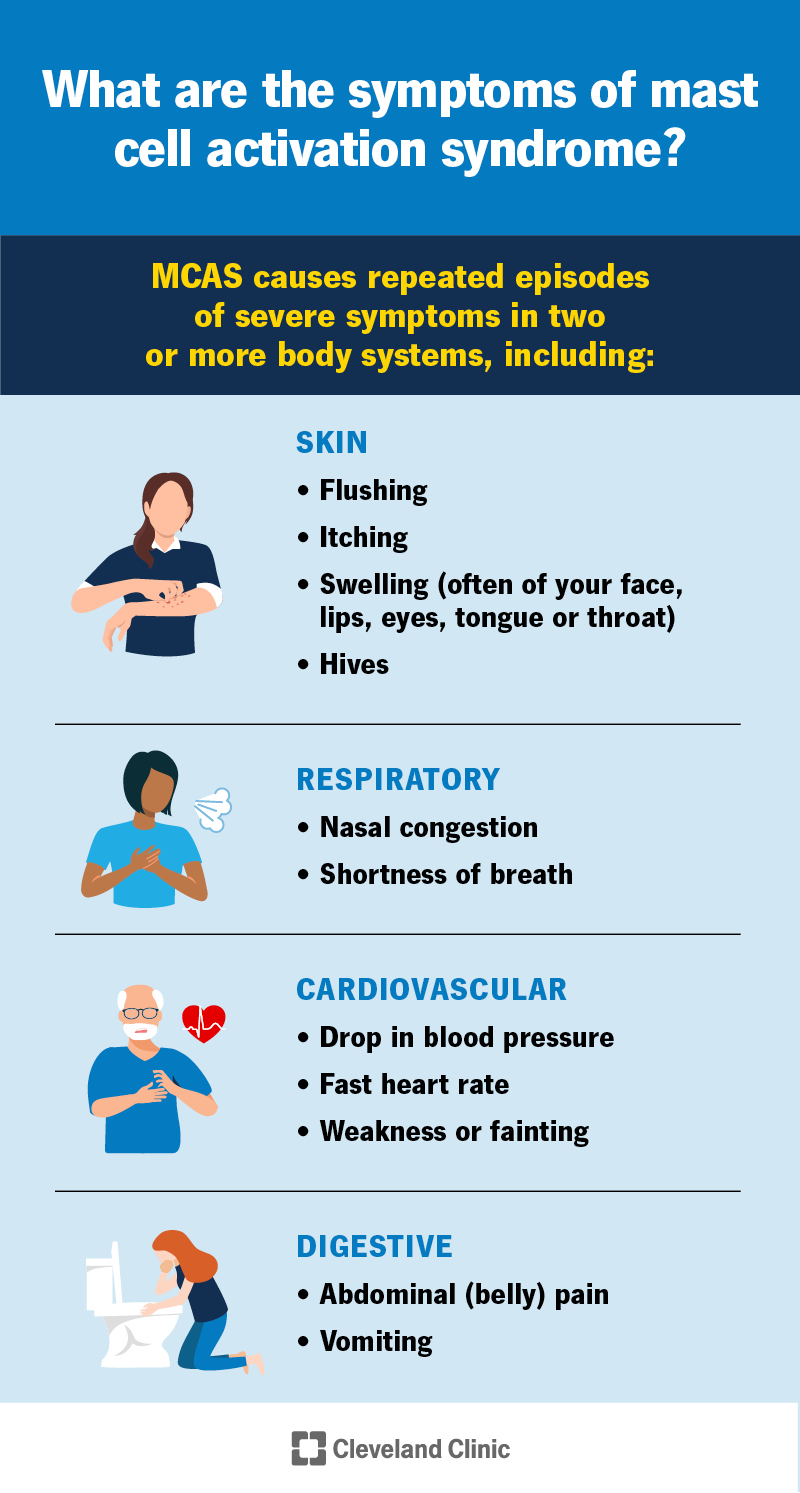
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/mcas)
Mast cell activation syndrome (MCAS) is when you have unexplained episodes of severe symptoms like swelling, diarrhea, vomiting, flushing and itching. Unlike allergies that happen with a specific exposure, MCAS episodes happen without a clear trigger.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In some cases, mast cell activation can cause anaphylaxis, a severe allergic condition that can be life-threatening. It can cause you to have trouble breathing and drop your blood pressure to dangerously low levels. Call 911 (or your local emergency service number) or go to the nearest emergency room if you’re experiencing severe anaphylaxis.
Mast cells are a type of immune cell responsible for immune reactions. For instance, conditions like allergic rhinitis and asthma, allergic reactions (like anaphylaxis to drugs or food) and mastocytosis all activate mast cells. This causes them to release proteins that give you symptoms that are bothersome at best, and dangerous at worst.
Other common conditions can also cause unexplained symptoms. It’s important to discuss your concerns with your provider. They’ll make sure you get a complete workup with a specialist, like an allergist. An allergist is a type of doctor who can diagnose and manage many types of allergic conditions.
But mast cell activation syndrome is rare. Healthcare providers diagnose mast cell activation syndrome if:
Advertisement
Mast cells are a part of your immune system. Their usual function is to help protect your body from invading germs (pathogens — like parasites or viruses) or other harmful substances. They sit in your tissues. When they recognize something they think is harmful, they release histamine and other chemicals to activate your immune system and try to flush out the intruder.
MCAS causes repeated episodes of severe symptoms in multiple areas of your body. Symptoms may include:
To be considered MCAS, the symptoms must affect two or more body systems. These include your:
If you’ve ever had an allergic reaction, you know what mast cell activation feels like. But for people with MCAS, episodes are often more severe than typical allergic reactions, and they involve multiple parts of the body. Your skin might get swollen and red, itch or break out in hives. You might get diarrhea or vomit. In extreme cases, the reaction is so severe that it can cause potentially life-threatening symptoms. Call 911 (or your local emergency service number) or go to the nearest emergency room if you’re experiencing severe symptoms.
Your mast cells reacting when they shouldn’t causes MCAS. Mast cells release proteins that cause your symptoms when they think they need to protect you from something harmful that’s entered your body. With allergies, you can identify something specific that causes your body to overreact. In MCAS, there doesn’t seem to be a clear trigger that causes your mast cells to release proteins.
No one’s really sure what causes your mast cells to get sensitive to things they shouldn’t be.
While many things can trigger mast cells to activate and release histamine (like food or pollen allergies), MCAS causes severe symptoms that aren’t predictably triggered by anything specific. You might find that you’re more likely to have episodes when you’re experiencing changes in your life or environment, like periods of high stress or shifting weather. If you find that episodes only happen after exposure to something specific, it’s not likely that you have MCAS.
A healthcare provider might think you have mast cell activation syndrome based on a physical exam, discussion of your symptoms and your medical history. Providers diagnose mast cell activation syndrome if you:
Advertisement
To test for MCAS, your provider may order a blood test to look for a sign of mast cell activation called tryptase. You have to get tested multiple times to check your levels, both when feeling well and when you’re having an episode. Keep in mind that tryptase can be elevated in other conditions, so tryptase levels alone don’t indicate MCAS. Some people naturally have higher-than-expected tryptase levels without symptoms.
Your provider may also do an allergy skin test or allergy blood tests to rule out other causes of your symptoms.
Healthcare providers don’t diagnose mast cell activation syndrome based on a histamine blood test. Elevated histamine levels don’t mean you have MCAS.
Providers use treatment to both diagnose MCAS and reduce your symptoms. If you don’t improve after treatment with mast cell-targeted medications, you probably don’t have MCAS.
Depending on your symptoms, your provider might prescribe:
Advertisement
Ways to take care of yourself with MCAS include:
Severe reactions due to MCAS are rare. But if you have symptoms of a serious allergic reaction or anaphylaxis and you have an epinephrine injector, use it. Then, call 911 (or your local emergency service number) or go to the nearest emergency room. Symptoms of anaphylaxis may include:
It might be helpful to ask your healthcare provider:
No, there’s no cure for MCAS. If you have MCAS, you’ll need to manage it with medications.
Advertisement
Providers expect that most people with MCAS live as long as someone without it. But it’s a newly recognized condition, so we can’t know for sure how it impacts life expectancy.
No, MCAS isn’t an autoimmune disorder.
Sirens are going off. Security’s on its way. Your mast cells have detected danger and have signaled for help. Except…there is no danger. Like an obnoxious prankster, your mast cells keep pulling the alarm when there’s no emergency. Instead of preventing you from getting sick, they’re the ones making you sick.
MCAS is rare. In most cases, other conditions are causing the symptoms. It’s important to talk to a provider to make sure you get the correct diagnosis.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.