Hypochondroplasia is a genetic condition that affects bone growth in your arms and legs. It leads to short stature. Hypochondroplasia is a mild form of achondroplasia. Children may develop defining physical characteristics like a curved spine and bowed legs as they grow. There’s no cure for the condition but treatment is available if you need it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Hypochondroplasia is a type of skeletal dysplasia or a condition that affects cartilage. Cartilage is connective tissue that protects your bones. It results in short-limbed dwarfism.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
For hypochondroplasia, a genetic change prevents cartilage from turning into bone (ossification) in the long bones in your arms and legs.
Physical characteristics of the condition include short stature, bowed legs and broad hands and feet along with a larger head size. Symptoms are rarely noticeable until toddlerhood to early school-age years.
The exact frequency of hypochondroplasia is unknown. Studies show that hypochondroplasia may occur at a similar rate as achondroplasia, which is a more severe form of the condition. The estimated rate of occurrence is 1 in 15,000 to 40,000 newborns around the world.
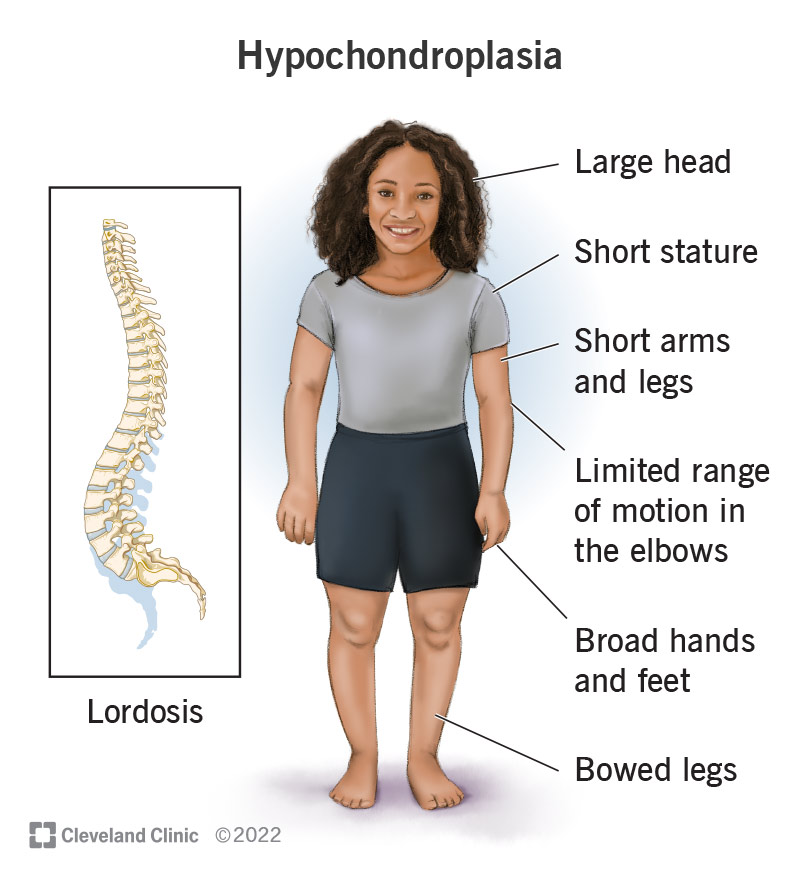
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/hypochondroplasia.jpg)
Several physical characteristics lead to a hypochondroplasia diagnosis. Symptoms vary from person to person and could include:
Growth (height) tends to decrease in toddlerhood to early school-age years. The average height for an adult diagnosed with hypochondroplasia is 138 cm (centimeters) to 165 cm (54 inches to 65 inches tall) for males and 128 cm to 151 cm (50 in to 59 in tall) for females.
You may experience joint pain in your arms and legs during your lifetime, especially after exercise or physical activity.
Advertisement
Although rare, fewer than 10% of people diagnosed with hypochondroplasia have mild intellectual challenges and problems learning through childhood and adolescence. Hypochondroplasia doesn’t usually affect your intelligence.
Short stature often goes unnoticed until early childhood when toddlers miss growth development milestones or adolescents don’t experience a growth spurt.
A genetic change (mutation) causes hypochondroplasia. Almost all cases occur because of a genetic change of the FGFR3 gene. The FGFR3 gene is responsible for creating a protein that develops and maintains how bones grow, especially during the conversion of cartilage (the soft connective tissue between bones) into bone. When the FGFR3 gene changes, proteins become overactive and can’t do their job to help bones grow and develop.
You can inherit hypochondroplasia in an autosomal dominant pattern. This means that only one biological parent needs to pass the gene change on to their child during conception to inherit it. So if one parent has it, there’s a 50% chance to pass it on. But most genetic mutations of the FGFR3 gene occur randomly, without being present in a person’s family history (de novo).
A small minority of cases of hypochondroplasia occur without a mutation of the FGFR3 gene. The cause is likely from a mutation of another, unidentified gene.
Hypochondroplasia can happen to any child. You might inherit the gene change from a biological parent or the change happens randomly. Genetic changes aren’t the result of something a parent did while pregnant. The occurrence is unpredictable.
A healthcare provider will diagnose hypochondroplasia after your baby is born. This happens because evidence of the condition isn’t always noticeable during a pregnancy ultrasound. If a mother has hypochondroplasia and the genetic cause is known, CVS (chorionic villus sampling) or amniocentesis would be options to diagnose the condition during pregnancy.
After birth, your provider will perform a physical examination of your child, along with a genetic test to pinpoint the gene that is responsible for symptoms.
Your healthcare provider will offer several tests to confirm the diagnosis of hypochondroplasia, including:
Treatment addresses the symptoms of hypochondroplasia that may lead to complications, like abnormal bone growth. Treatment is different for each person and could include:
Advertisement
Some families and people diagnosed with hypochondroplasia benefit by joining support groups to talk about their (or their child’s) diagnosis among peers who share a similar experience. Support groups offer helpful information like education on employment, disability rights and parenting.
Hypochondroplasia is a lifelong condition with no cure. It doesn’t affect your child’s life expectancy and they’ll have a normal lifespan.
Symptoms of your child’s diagnosis usually aren’t noticeable until they reach early adolescence (they won’t experience a growth spurt). This means they’ll be shorter than their peers.
It’s common for children to experience minor aches or mild pain in their knees, elbows and ankles after exercise. Long-term joint discomfort and pain can occur through adulthood.
Your child’s healthcare provider will track their growth during routine examinations and offer treatment options to manage your child’s symptoms as they arise.
Since hypochondroplasia is the result of a genetic change that occurs randomly, there isn’t a way to prevent the condition unless a couple undergoes preimplantation genetic testing.
Advertisement
Your risk of having a child with a genetic condition increases if you smoke or have chemical exposure during pregnancy.
If you plan on becoming pregnant, talk with your healthcare provider to learn about your risk of having a child with a genetic condition.
If your child diagnosed with hypochondroplasia experiences symptoms of the condition that prevent them from accomplishing their daily tasks or they experience severe pain, especially in their arms and legs, you should contact your healthcare provider.
Also, let your provider know if your child misses developmental milestones for their age — like having a growth spurt, for example, if they don’t have a hypochondroplasia diagnosis.
Questions you may want to ask your healthcare provider include:
Both hypochondroplasia and achondroplasia are genetic conditions caused by the FGFR3 gene. They affect a person’s bone growth and height. Hypochondroplasia is a mild form of achondroplasia, where symptoms are less severe.
Children diagnosed with hypochondroplasia usually won’t miss out on everyday childhood activities as a result of their diagnosis. For many children, they’re just shorter than their peers but don’t experience any life-altering symptoms. They may be more at risk of bullying as they go through school, so offer support and talk to a mental health professional if necessary. It’s common for families with a child diagnosed with hypochondroplasia to reach out to support groups to connect with others and learn from their experiences.
Advertisement
If you plan on becoming pregnant and want to understand your risk of having a child with a genetic condition, reach out to your healthcare provider to discuss genetic testing.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
As your child grows, you need healthcare providers by your side to guide you through each step. Cleveland Clinic Children’s is there with care you can trust.
