Bacterial vaginosis (BV) is a common vaginal infection that happens when some normal bacteria that live in your vagina overgrow, causing a bacterial imbalance. Symptoms include an off-white or gray vaginal discharge that smells “fishy.” BV is easily treatable with antibiotics from a healthcare provider.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
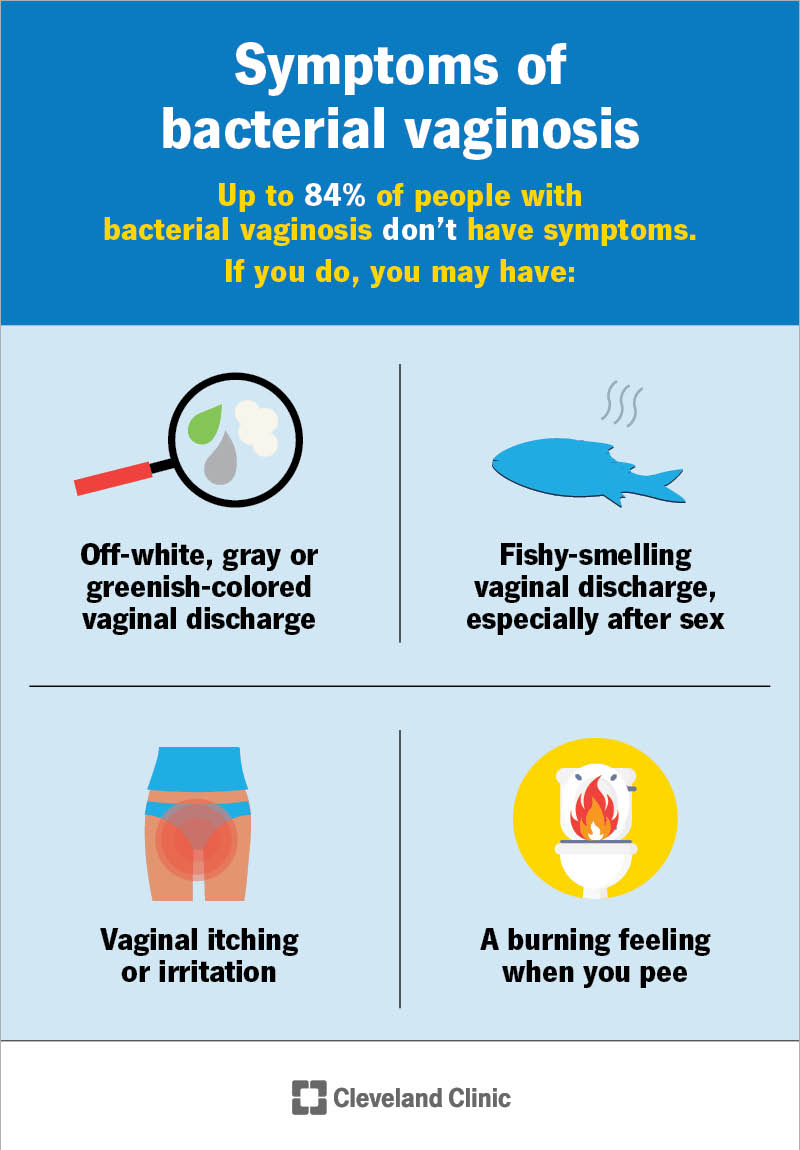
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/3963-bacterial-vaginosis)
Bacterial vaginosis (BV) is a vaginal infection caused by an overgrowth of bacteria. Every healthy vagina contains bacteria. Typically, these bacteria balance each other. Sometimes, the “bad” bacteria grow too much and overpower the “good” bacteria. This throws off the balance of bacteria in your vagina and leads to bacterial vaginosis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Bacterial vaginosis may cause your vaginal discharge to have a “fishy” odor. It can also cause vaginal irritation in some people. Others may not have any symptoms of BV.
Bacterial vaginosis is the most common vaginal problem for women ages 15 to 44. In fact, about 35% of people with a vagina will get BV. The rate is higher if you’re Black.
Anyone with a vagina can get bacterial vaginosis. It usually occurs in people who are sexually active. It’s rare for it to occur in people who’ve never had sex. Some people may naturally produce too much of the bacteria that causes BV.
You may have a higher risk of getting BV if you:
Up to 84% of people with bacterial vaginosis don’t have symptoms. If you do, you may have:
BV symptoms are similar to other infections. It’s important to visit a healthcare provider to determine if what you have is BV or another vaginal infection.
Advertisement
Your vagina is home to multiple types of bacteria (called a microbiome). A change in the balance of the bacteria causes BV.
Specifically, bacterial vaginosis happens when “bad” bacteria (anaerobes) grow more quickly than “good” bacteria (lactobacilli). Too much of one type of bacteria leads to an imbalance.
Researchers know that anything that changes the natural chemistry of your vagina can affect the bacteria in your vagina. That’s why certain activities like douching or unprotected sex can lead to BV. You can’t get BV from hot tubs, swimming pools or toilet seats. You also can’t get BV from touching a surface that a person with BV has touched.
Bacterial vaginosis doesn’t spread from person to person, but sexual activity can increase your risk of getting the infection.
Bacterial vaginosis isn’t sexually transmitted, but it’s linked to sexual activity. Researchers think that sex may change the bacterial environment in your vagina. This makes bacterial overgrowth more likely.
Both bacterial vaginosis and yeast infections are vaginal infections that increase amounts of discharge. Here’s how you can tell the difference:
Only a healthcare provider can diagnose bacterial vaginosis. Contact a provider for an appointment if you have signs of BV. At your appointment, your provider will ask you about your medical history, including vaginal infections or sexually transmitted infections (STIs). They may also:
Tests for bacterial vaginosis use samples of fluid from your vagina. That sample can undergo several types of tests for bacterial vaginosis. The most common are:
Your healthcare provider will prescribe antibiotics, typically metronidazole or clindamycin. These medications come in a gel or cream you insert into your vagina. Some antibiotics are pills you can take orally (by swallowing them).
Advertisement
It’s important to finish the antibiotic and take it as your provider prescribes. Stopping early because your symptoms go away increases your risk of getting BV again.
Some cases of bacterial vaginosis resolve on their own without any medications. However, if you have symptoms, you should seek medical care. Having BV makes you prone to sexually transmitted infections and can affect pregnancy.
There are no over-the-counter products to treat bacterial vaginosis (BV). Avoid using douches or products meant for yeast infections, which could make BV worse. See a healthcare provider for treatment.
Most of the time, one round of antibiotics — taken for up to seven days — eliminates the infection. About 10% to 15% of people need another round of treatment.
Yes. Up to 80% of people get bacterial vaginosis again in their lifetime.
Bacterial vaginosis doesn’t typically cause serious complications. But if left untreated it could lead to:
Advertisement
You can’t prevent bacterial vaginosis. However, taking these precautions could reduce your risk:
If BV keeps coming back, it may help to talk openly with your partner. In some cases, working with a certified sex therapist can improve communication, address concerns about intimacy and support healthy sexual habits that may reduce recurrence.
If you have bacterial vaginosis (BV), your provider can prescribe medication that’s safe to use during pregnancy. You should get treated for the infection whether or not you have symptoms. BV can cause pregnancy complications, such as premature birth or having a baby that weighs less than average (low birth weight).
Advertisement
Men don’t need to be treated for bacterial vaginosis (BV). If you have a female partner, they may have BV, too. It’s important to let them know so they can get treatment.
Call your provider if you have:
No. But you can spread the bacteria that causes BV. So, this means you can get BV from a female partner and spread it to another female partner.
Yes. If one partner has BV, there are steps you can take to protect yourself.
Yes. About 25% of pregnant women will get BV. This is due to all the hormonal changes that occur in pregnancy.
Although bacterial vaginosis (BV) is a mild infection, it can make you vulnerable to more serious conditions. Don’t put off seeing a healthcare provider if you notice anything unusual about your vaginal discharge. Your provider can treat BV with antibiotics.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have vaginitis, getting relief from your discomfort is probably top of mind. Cleveland Clinic’s experts can craft a treatment plan that works for you.
